Session Information
Date: Saturday, November 12, 2022
Title: Vasculitis – ANCA-Associated Poster I: Epidemiology, Outcomes, and Classification
Session Type: Poster Session A
Session Time: 1:00PM-3:00PM
Background/Purpose: Anti-neutrophil cytoplasmic antibody( ANCA)-associated vasculitis, characterized by inflammation of small and medium sized blood vessels includes three main conditions – eosinophilic granulomatosis with polyangiitis, granulomatosis with polyangiitis and microscopic polyangiitis. Due to the chronic inflammation associated with the disease process as well as use of cytotoxic drugs, it may be associated with potential cardiovascular complications. The aim of our study is to evaluate the cardiovascular conditions in patients with ANCA-associated vasculitis along with sex based differences in cardiovascular conditions.
Methods: All patients were included who were diagnosed with ANCA-associated vasculitis between January 1, 2016 and December 31, 2019 with age more or equal to 18 years in the National Inpatient Sample, the largest all-payer public database of hospital care data in the United States using ICD 10 diagnosis codes. Associated demographics, comorbidities, and hospital complications were extracted from the hospitalization record and reported descriptively. Fisher’s exact test compared sex-specific differences in cardiovascular complications.
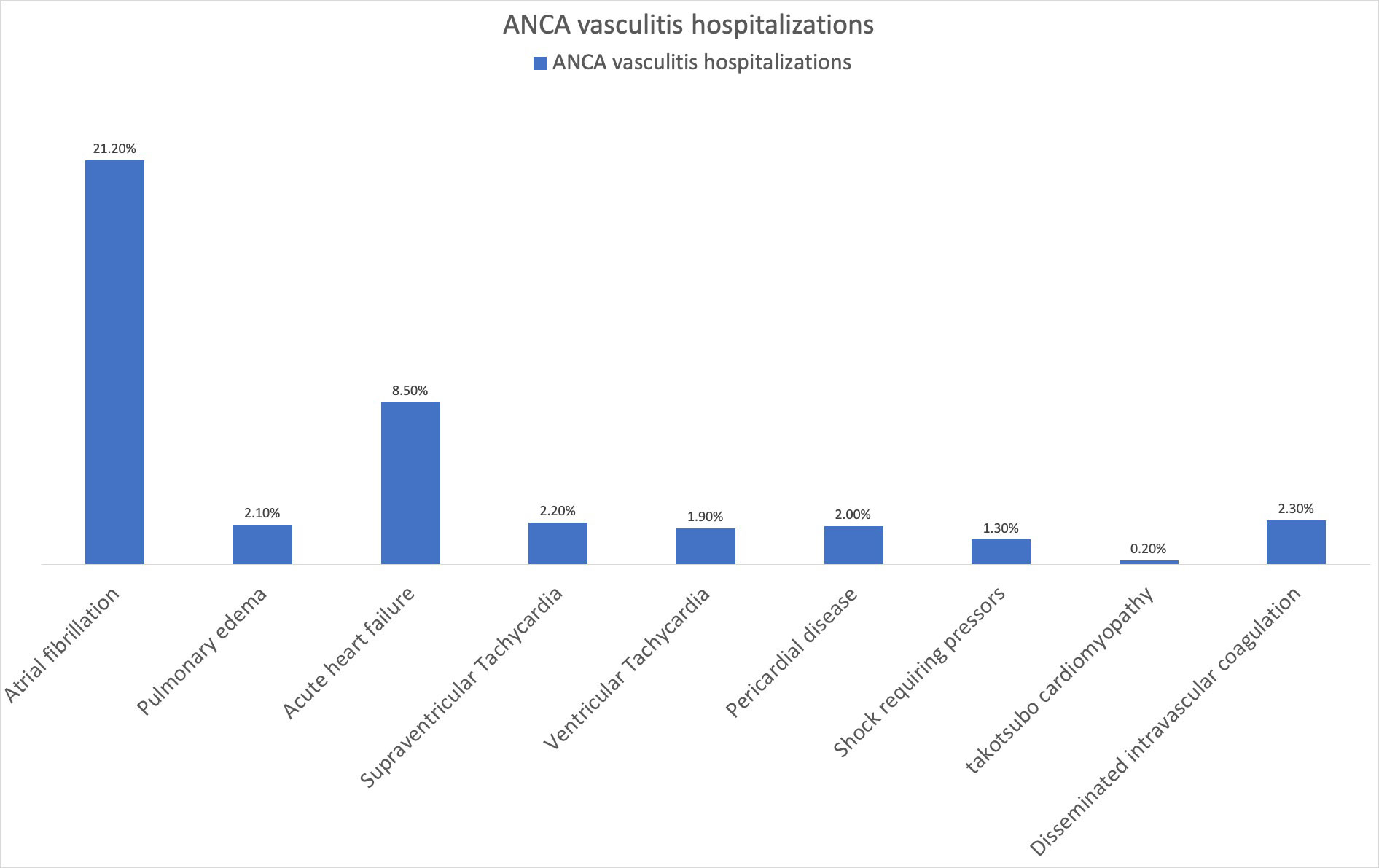
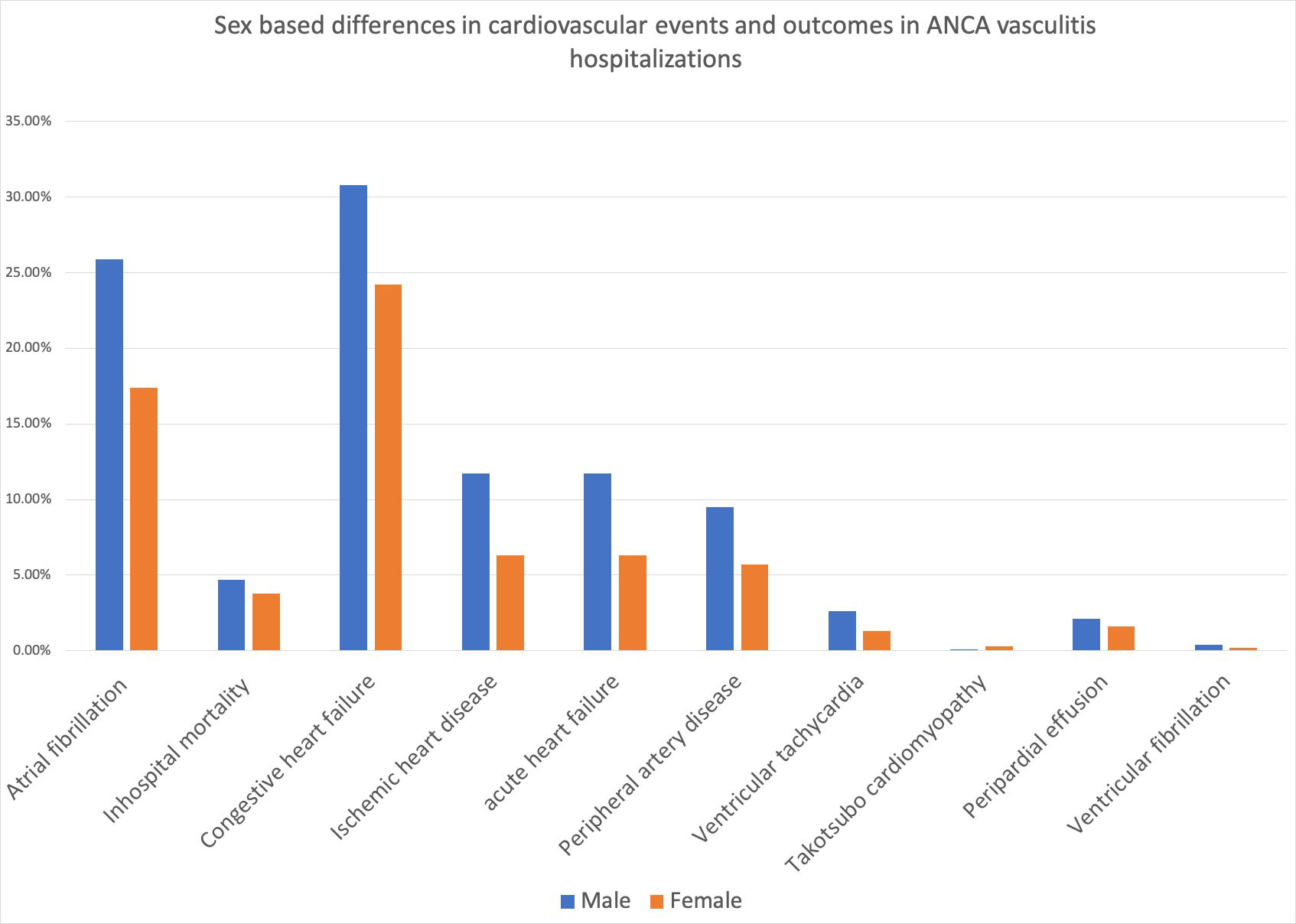
Results: From 2016 to 2019, among a total of 28,48,4087 hospitalizations (unweighted sample), 12,306 admissions (45.2 % male, mean age 62.4 ± 16.5 years) included ANCA-associated vasculitis. Among ANCA-associated vasculitis hospitalizations, racial distributions were White 74.5% , Black 7.9% , Hispanic 11.6%, and Asian 2.4%. 517 patients (4.2%) died in the hospital; mean length of stay (LOS) was 7.2 days. The most common comorbid cardiovascular diagnosis was atrial fibrillation (n=2614; 21.2%). Among ANCA vasculitis, 0.2% (n=22) had takotsubo cardiomyopathy, 2.1% (n=252) had pulmonary edema, 8.5% (n=1049) had acute decompensated heart failure, 2.2% (n=269) had supraventricular tachycardia, 1.9% (n=236) had ventricular tachycardia, 0.3% (n=33) had ventricular fibrillation, 2% (n=252) had pericardial disease (including acute or chronic pericarditis or tamponade), 1.3% (n=155) required pressors, and 2.3% (n=281) had disseminated intravascular coagulation. Among ANCA vasculitis, compared to males, females were younger in age (mean age: 62 vs. 63 years; p=0.011), had lower prevalence of atrial fibrillation (17.4% vs 25.9%, p< 0.001), congestive heart failure (24.2 % vs 30.8%, p< 0.001), ischemic heart disease (6.3% vs 11.7%, p< 0.001), peripheral vascular disease (5.7% vs 9.5%, p< 0.001), acute decompensated heart failure (7.4% vs 10%, p< 0.001), pericardial effusion ( 1.6% vs 2.1%, p=0.049), ventricular tachycardia (1.3% vs 2.6%, p< 0.001), ventricular fibrillation (0.2% vs 0.4%, p=0.014), and higher prevalence of takotsubo cardiomyopathy (0.3% vs 0.1%, p=0.01), had lower in-hospital mortality (3.8% vs 4.7%, p=0.010) and shorter length of stay (7 days vs 7.4 days, p=0.019).
Conclusion: Among ANCA-vasculitis hospitalizations, atrial fibrillation is the most common cardiovascular condition and females had fewer cardiovascular complications, lower in-hospital mortality and shorter length of stay compared to males.
To cite this abstract in AMA style:
bashyal K, Baral N, Ghimire C, Balmuri S, Kunadi A, Karki S. Sex Based Differences in Cardiovascular Conditions Associated with Anti-neutrophil Cytoplasmic Antibody-Associated Vasculitis: A Retrospective Analysis of the National Inpatient Sample [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/sex-based-differences-in-cardiovascular-conditions-associated-with-anti-neutrophil-cytoplasmic-antibody-associated-vasculitis-a-retrospective-analysis-of-the-national-inpatient-sample/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/sex-based-differences-in-cardiovascular-conditions-associated-with-anti-neutrophil-cytoplasmic-antibody-associated-vasculitis-a-retrospective-analysis-of-the-national-inpatient-sample/