Session Information
Session Type: Poster Session D
Session Time: 8:30AM-10:30AM
Background/Purpose: Severity factors for COVID-19 have been widely studied in the general population. However, the severity factors and characteristics of COVID-19 in patients with rheumatic immune-mediated inflammatory diseases (R-IMID) remain unknown. Our aim was to analyze the severity factors of COVID-19 infection in R-IMID.
Methods: Cross-sectional study in a single University Hospital. We included all consecutive patients with a diagnosis of a R-IMID and a positive test for COVID-19 up to March 31st, 2021. Confirmed infection was defined if the patient had a positive nasopharyngeal swab for SARS-CoV-2. Medical records of 25,367 patients that suffered COVID-19 in our region, and 7,218 with R-IMID from our hospital were reviewed. COVID-19 severity was divided into mild, moderate, severe and critical according to the United States National Institute of Health (NIH) COVID-19 guidelines. Mild/moderate COVID19 was compared to critical.
Results: We included 274 patients (185 women/89 men), mean age 59.1±18 years. Most cases were mild to moderate (n=245). The remaining patients presented severe (n=8) or critical (n=21) disease. 17 (6.2%) presented a fatal outcome.
More frequent R-IMID were: Rheumatoid arthritis (RA) (n=87, 31.8%), Axial spondyloarthritis/ Psoriatic arthritis (SpA/PsA) (n=90, 32.8%), Polymyalgia Rheumatica (PMR) (n=22, 8%) and Systemic Lupus Erythematosus (SLE) (n=22, 8%) (FIGURE).
Main comorbidities were hypertension (n=119, 43.4%), dyslipidemia (n=119, 43.4%), age higher than 65 years old (n=100, 36.5%), obesity (n=49, 17.9%), cardiovascular disease (n=45, 16.4%), diabetes mellitus (n=36, 13.1%), chronic pulmonary disease (n=29, 10.6%) and chronic kidney disease (n=27, 9.9%).
Comorbidities in R-IMID associated with severe to critical disease (p< 0.05) were hypertension, dyslipidemia, age higher than 65 years, previous cardiovascular, kidney or lung disease and PMR.
Rituximab was the only treatment associated with increased severity of COVID-19 (p <0.05). Severe/critical compared with mild/moderate disease showed significantly higher levels of serum creatinine, and lower levels of lymphocytes and received more frequently systemic glucocorticoids (TABLE). Tocilizumab and Anakinra were used only in critical patients, 2 cases each.
Conclusion: Although most cases of COVID-19 are mild, it can be a life-threatening disease in patients with R-IMID. Hypertension, dyslipidemia, older age, previous cardiovascular, kidney or lung disease, the use of rituximab and PMR were associated with critical disease.
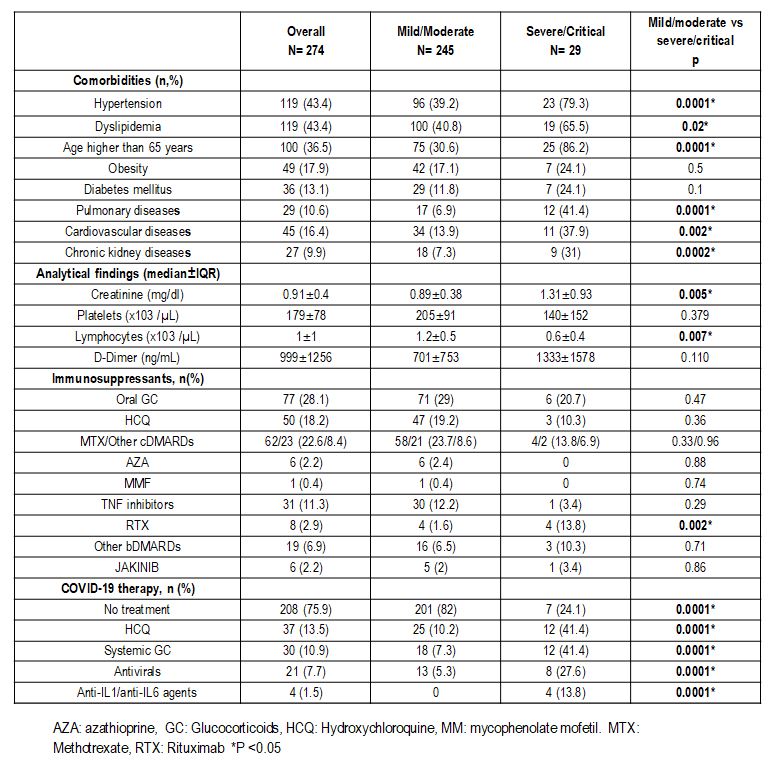 TABLE. Clinical severity of 274 with R-IMID diagnosed with COVID_19 (analytical findings and Immunosuppressants are at COVID diagnosis).
TABLE. Clinical severity of 274 with R-IMID diagnosed with COVID_19 (analytical findings and Immunosuppressants are at COVID diagnosis).
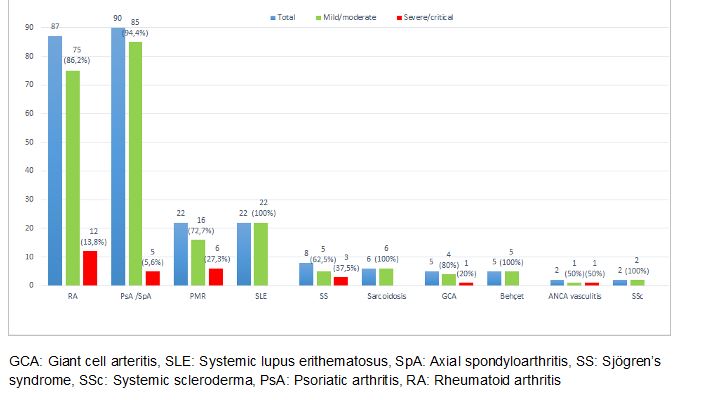 FIGURE: Severity of COVID_19 according to R-IMID. Data between parentheses are the percentage of patients with mild/moderate or severe/critical disease.
FIGURE: Severity of COVID_19 according to R-IMID. Data between parentheses are the percentage of patients with mild/moderate or severe/critical disease.
To cite this abstract in AMA style:
Martinez-Lopez D, Prieto-Peña D, Sánchez-Bilbao L, Álvarez-Reguera C, Herrero-Morant A, Benavides-Villanueva F, Corrales-Selaya C, Trigueros-Vazquez M, gonzalez-Gay M, Blanco R, Wallmann R. Severity Factors of Covid-19 Infection in Rheumatic Immune-mediated Inflammatory Diseases: Study in a Single University Hospital [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/severity-factors-of-covid-19-infection-in-rheumatic-immune-mediated-inflammatory-diseases-study-in-a-single-university-hospital/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/severity-factors-of-covid-19-infection-in-rheumatic-immune-mediated-inflammatory-diseases-study-in-a-single-university-hospital/
