Session Information
Date: Sunday, November 10, 2019
Title: 3S100: B Cell Biology & Targets in Autoimmune & Inflammatory Disease (880–885)
Session Type: ACR Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: Tubulointerstitial inflammation (TII) in lupus nephritis (LN) is associated with a worse prognosis. Vimentin, a cytoplasmic antigen, is commonly targeted by in situ activated B-cells in TII. The prognostic importance of high serum anti-vimentin antibodies (AVAs) in LN and their relationship with common lupus autoantibody specificities is unknown. We investigated associations between AVA isotypes, other autoantibodies, and response to mycophenolate mofetil in the presence or absence of rituximab.
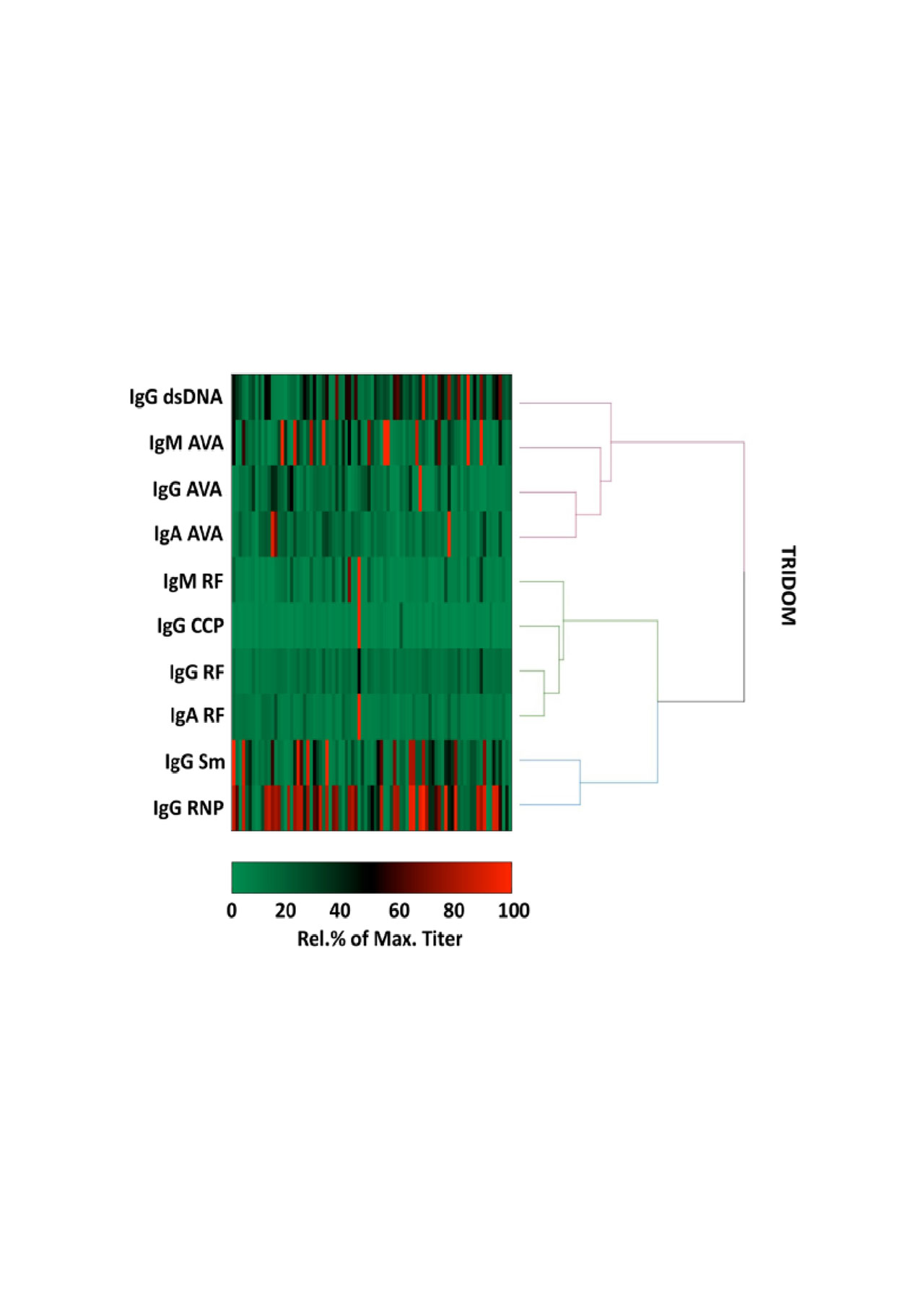
Methods: An inhouse AVA ELISA was developed using human vimentin as substrate (over expressed in, and purified from the inclusion bodies of, E.coli). Serum from a cross-sectional cohort of 99 lupus patients (22% LN, from the Translational Research Inititative in the Department of Medicine, “TRIDOM”) was titrated for IgG-, IgA- and IgM- AVAs, lupus- associated, and RA-associated autoantibodies, and titers subjected to hierarchical clustering. Serum from baseline, 26 and 52 weeks from 131 proliferative LN patients enrolled in the LUNAR trial was analysed for a more exhaustive range of lupus associated antibodies and evaluated for associations with longitudinal laboratory parameters up to week 78.
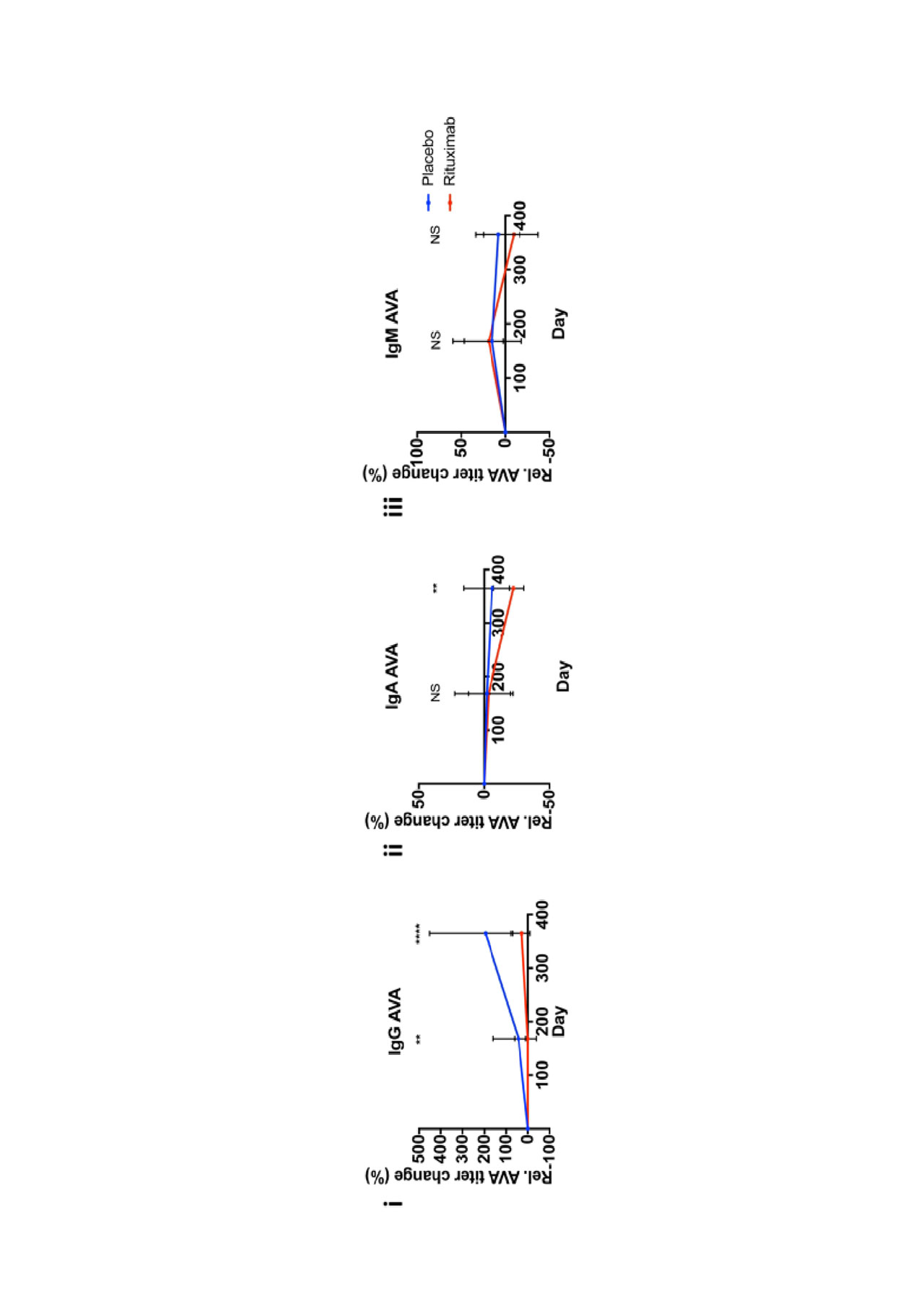
Results: In TRIDOM, hierarchical clustering analysis revealed AVAs and IgG anti-dsDNA clustered together, whereas AVAs clustered away from anti-Sm, anti-RNP, and RA-associated autoantibodies. In LUNAR at baseline, AVAs correlated weakly with anti-dsDNA and more strongly with anti-cardiolipin titers. IgG anti-dsDNA titers were reduced in both treatment groups, but more profoundly in patients receiving rituximab. In contrast, IgG AVAs increased in both treatment groups from baseline to week 52 (median fold increase of 195% in the absence vs 28% in the presence of rituximab) while titers of IgM and IgA AVAs did not increase over time. Over 78 weeks a reduction in proteinuria was observed for each treatment group, as reported previously at 52 weeks. However, less reduction in proteinuria was observed for patients with baseline high titers of IgG AVA (p< 0.0001 for overall effect; mean difference in change of UPCR between high and low groups at week 78 = 1.42 g/g) and IgA AVA (p=0.0069; mean difference: 0.88 g/g). In comparison, baseline IgM AVA status was not associated with subsequent difference in change of UPCR (p=0.75).
Conclusion: AVAs, especially IgG AVAs, are unique in distribution and response to therapy compared to other commonly measured autoantibody specificities in lupus. Furthermore, high-titer IgG AVAs identify LN patients resistant to conventional therapies. AVAs may represent a new class of prognostic autoantibodies.
To cite this abstract in AMA style:
Kinloch A, Cascino M, Dai J, Bermea R, Ko K, Vesselits M, Legendre M, Okoreeh M, Markovitz D, Dragone L, Townsend M, Clark M. Serum Anti-Vimentin Autoantibodies May Uniquely Predict Response to Therapy in Lupus Nephritis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/serum-anti-vimentin-autoantibodies-may-uniquely-predict-response-to-therapy-in-lupus-nephritis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/serum-anti-vimentin-autoantibodies-may-uniquely-predict-response-to-therapy-in-lupus-nephritis/