Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Previous studies have demonstrated that the presence of autoantibodies against N-methyl-D-aspartate (NMDA) receptor subunit 2 (NR2) is closely associated with brain damages leading to the development of diffuse neuropsychiatric SLE (NP-SLE). NR1 is another subunit forming functional NMDA receptor with NR2. However, it is not clear whether anti-NR1 antibodies (anti-NR1) might be expressed in SLE. Nor has their role in the pathogenesis in NP-SLE been clarified. The present study therefore explored the serum levels of anti-NR1 in SLE.
Methods: Sera were obtained from 108 patients with SLE, 36 various rheumatic diseases other than SLE (7 patients with RA, 8 with Behcet’s disease, 3 with vasculitis syndromes, 6 with SSc, 6 with PM/DM and 6 with MCTD) and 91 healthy individuals. Among the 108 SLE patients, 67 showed neuropsychiatric manifestations. IgG anti-NR1 antibodies were measured by ELISA, using the N-terminal 100-amino acid of murine NR1, which is more than 90% homologous to human NR1. The results were reported as arbitrary units determined using a positive serum. Some sera positive for anti-NR1 were further analyzed for the fine epitopes they recognize, using 4 different preparations of synthetic 25 amino-acid sequences within the N-terminal 100 amino-acid sequence of human NR1.
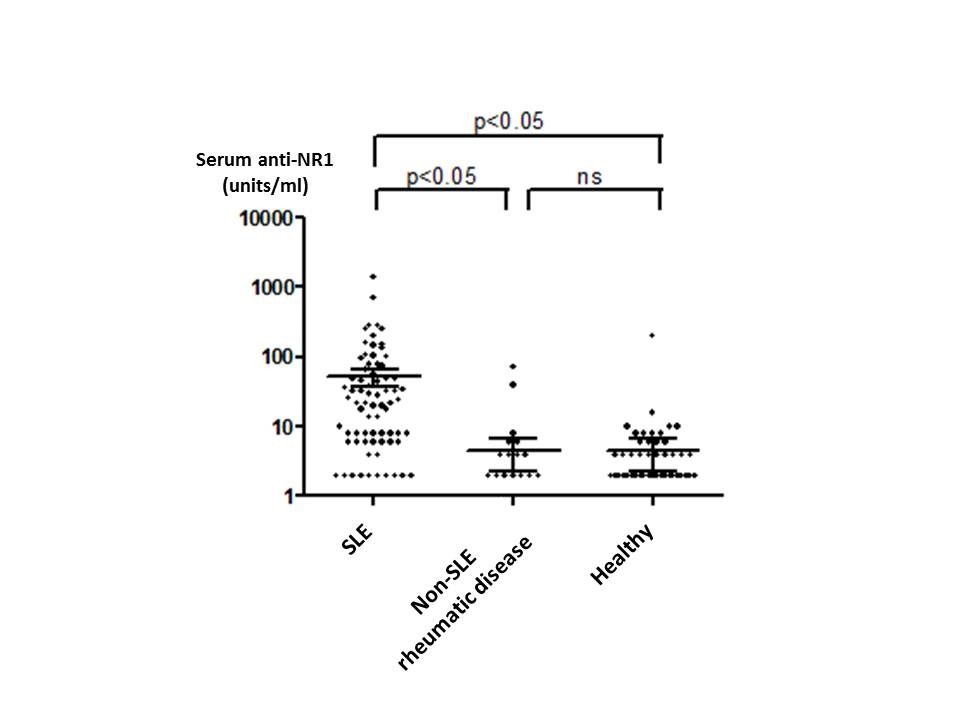
Results: The mean ± SEM values for serum anti-NR1 in 91 healthy individuals were 4.48 ± 2.19 units/ml. Serum anti-NR1 levels were significantly elevated in SLE (52.18 ± 15.22 units/ml) compared with healthy individuals or with non-SLE rheumatic diseases (4.50 ± 2.23 units/ml). There was no significant difference in serum anti-NR1 between non-SLE rheumatic diseases and healthy individuals. Of note, serum anti-NR1 were significantly higher in NP-SLE (74.60 ± 23.96 units/ml) than those in SLE without neuropsychiatric manifestations ((15.54 ± 5.62 units/ml) (p=0.044)). Finally, anti-NR1 bound most efficiently to the sequence of amino acids between position 57 and position 81 from the N-terminus of human NR1.
Conclusion: The results indicate that anti-NR1 were specifically elevated in SLE patients. Moreover, the data also suggest that anti-NR1 might be involved in the pathogenesis of NP-SLE, presumably through transudation through blood-brain barrier into CNS.
Disclosure:
O. Eisuke,
None;
N. Tatsuo,
None;
A. Yoshiyuki,
None;
H. Shunsei,
None.
« Back to 2012 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/serum-anti-n-methyl-d-aspartate-receptor-subunit-1-antibodies-are-elevated-in-sle/