Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: To study incidence, time-trends and outcomes of serious infections in systemic sclerosis (SSc).
Methods: We used the 1998-2016 U.S. National Inpatient Sample data. We examined the epidemiology, time-trends and outcomes of five serious infections (opportunistic infections (OI), skin and soft tissue infections (SSTI), urinary tract infection (UTI), pneumonia, and sepsis/bacteremia) in hospitalized people with SSc. We performed multivariable-adjusted logistic regression analyses to analyze independent association of factors with healthcare utilization (hospital charges, length of hospital stay, discharge to non-home setting), and in-hospital mortality.
Results: There were 49,904,955 hospitalizations with serious infections in people without SSc and 61,615 in those with SSc. The average age of patients with SSc with a serious infection was 61.4 years (median of 61.7 years; Table 1), similar to all SSc hospitalizations.
Compared to patients admitted with serious infection without SSc, people with SSc were younger (median age, 65 vs. 62 years), and were more likely to be female (52% vs. 84%), or have Deyo-Charlson score of 2 or more (42% vs. 64%; Table 1).
During 1998-2016, the most common serious infections in SSc were pneumonia (45%), sepsis (32%), SSTI (19%), UTI (3%) and OI (3%). In 2013-14, sepsis surpassed pneumonia as the most common serious infection; by 2015-16, sepsis was 1.8-times more common than pneumonia (Figure 1). Over the study period, hospital charges increased, while length of hospital stay and in-hospital mortality decreased, overall and for each serious infection.
Multivariable-adjusted analyses showed that sepsis, age ≥80 years and Deyo-Charlson score ≥2 were associated with significantly higher odds of healthcare utilization and in-hospital mortality; and Medicare or Medicaid insurance payer, Northeast location, urban teaching or non-teaching hospital, and medium or large hospital bed size with significantly higher odds of healthcare utilization (Table 2).
Conclusion: Outcomes in people with SSc hospitalized with serious infections have improved over time, except higher hospital charges. Identification of factors associated with higher healthcare utilization and in-hospital mortality allows for developing interventions to further improve these outcomes.
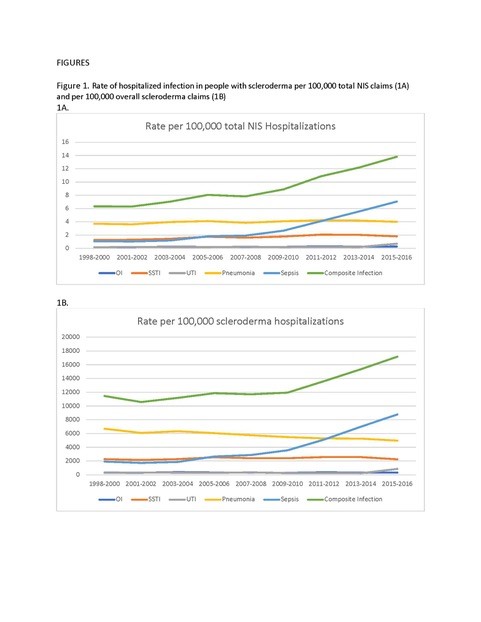 Figure 1. Rate of hospitalized infection in people with scleroderma per 100,000 total NIS claims (1A) and per 100,000 overall scleroderma claims (1B)
Figure 1. Rate of hospitalized infection in people with scleroderma per 100,000 total NIS claims (1A) and per 100,000 overall scleroderma claims (1B)
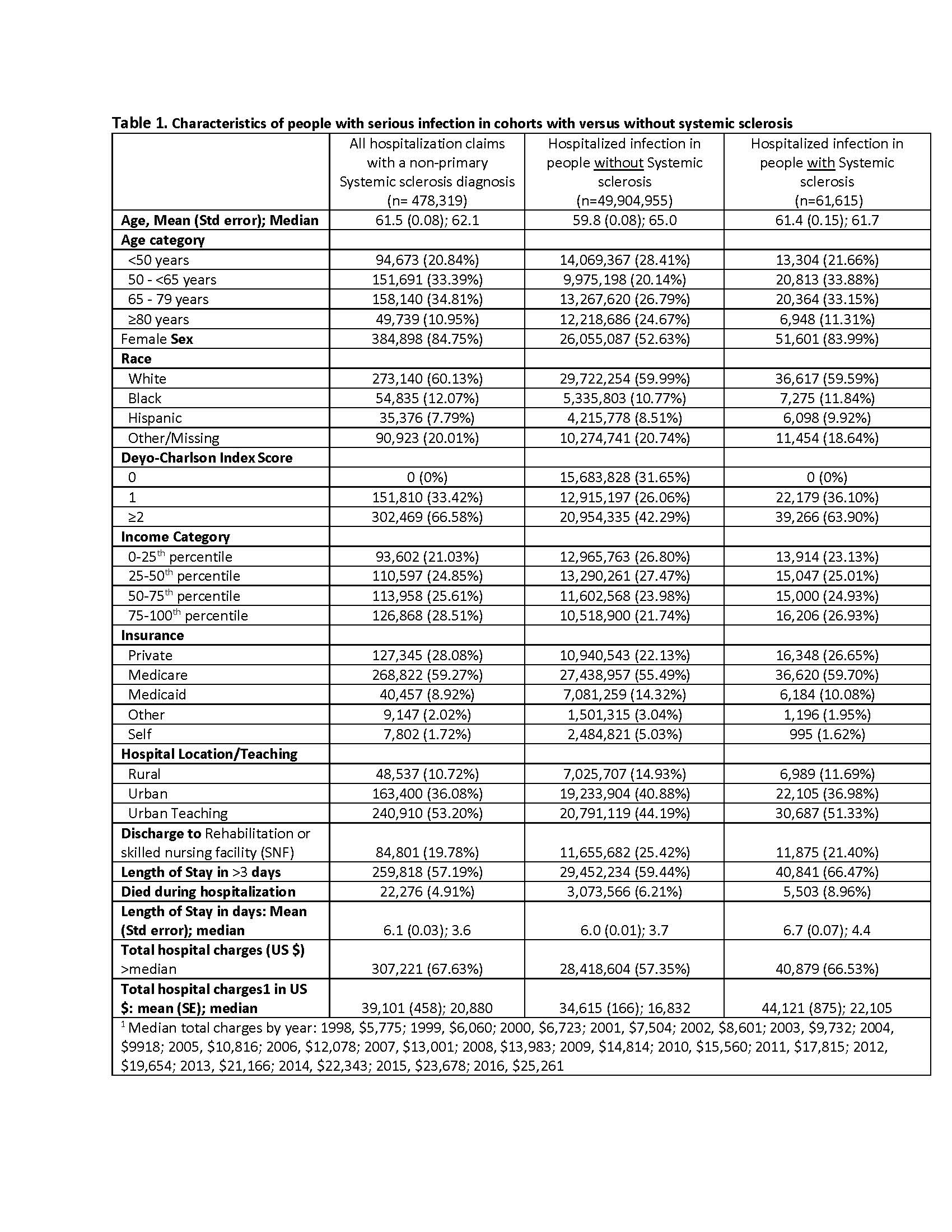 Table 1. Characteristics of people with serious infection in cohorts with versus without scleroderma
Table 1. Characteristics of people with serious infection in cohorts with versus without scleroderma
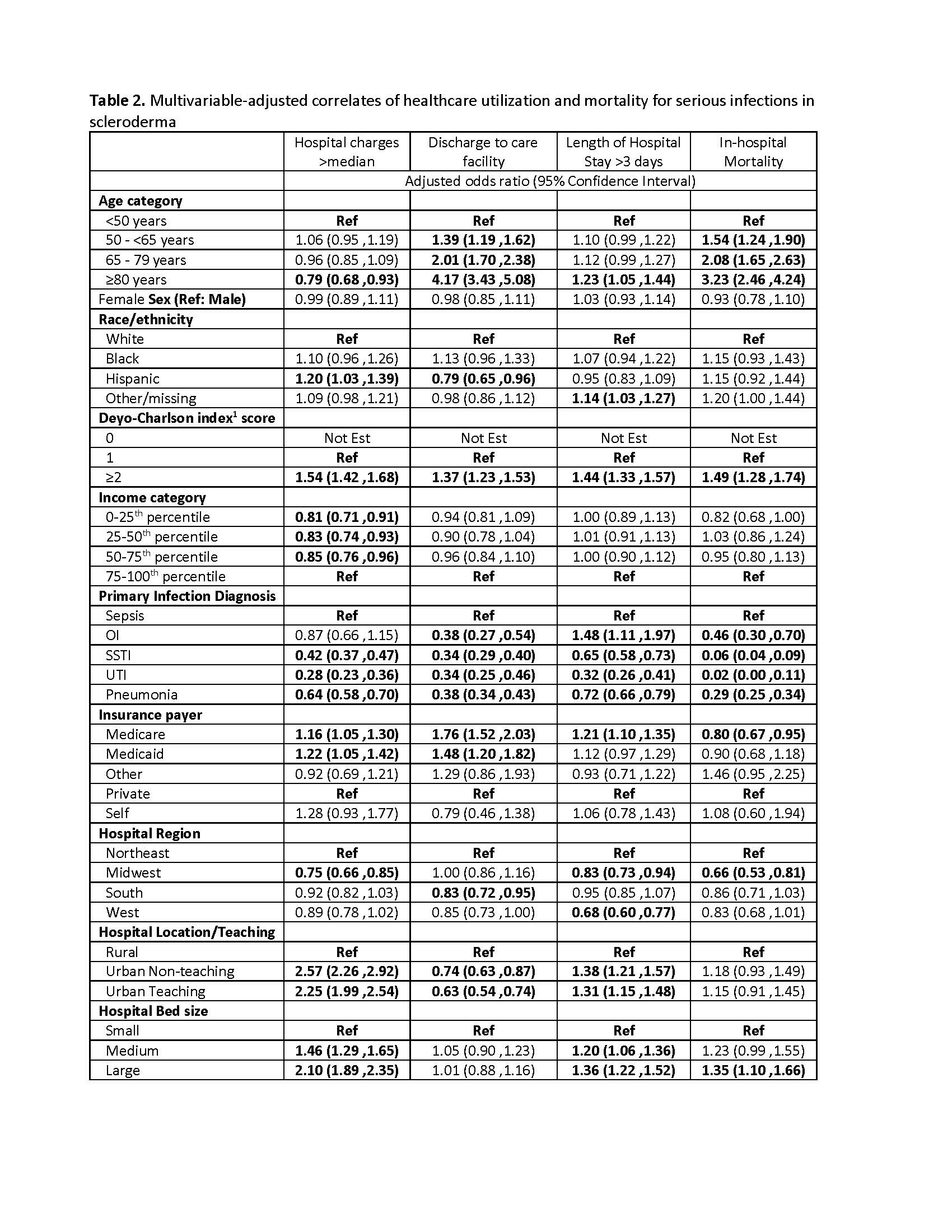 Table 2. Multivariable-adjusted correlates of healthcare utilization and mortality for serious infections in scleroderma
Table 2. Multivariable-adjusted correlates of healthcare utilization and mortality for serious infections in scleroderma
To cite this abstract in AMA style:
Singh J, Cleveland J. Serious Infections in People with Systemic Sclerosis: A National U.S. Study [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/serious-infections-in-people-with-systemic-sclerosis-a-national-u-s-study/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/serious-infections-in-people-with-systemic-sclerosis-a-national-u-s-study/
