Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Recent studies provide conflicting results on the impact of DMARDs on the risk of serious infections for patients with RA. We examined these infection risks by type, site, and treatment in a real world setting.
Methods: Participants were followed biannually from 1998 through 2013 in a large US longitudinal observational study. Serious infections were defined as those requiring hospitalization or intravenous antibiotics, or led to death within a year after the patient’s last observation. Infections were validated from hospitalization, physician, and death records. Infections were categorized as opportunist, by cause and by syndrome. Survival analysis methods (Cox regression, time to first infection using time-varying covariates and Andersen-Gill multiple failures model) were applied, both in a univariate and multivariate manner. Confounders included demographics, clinical status, disease severity and medications. DMARDs and biologics were grouped using different categorizations: methotrexate (MTX), non-MTX DMARDs (NMTX), anti-TNF (TNF), and no DMARD/biologic (nDB). Individual drugs included abatacept (ABA), adalimumab (ADA), etanercept (ETA), infliximab (INF), rituximab (RIT), and leflunomide (LEF). An at-risk window of 3 months was considered for all drugs (except RIT with 12 months).
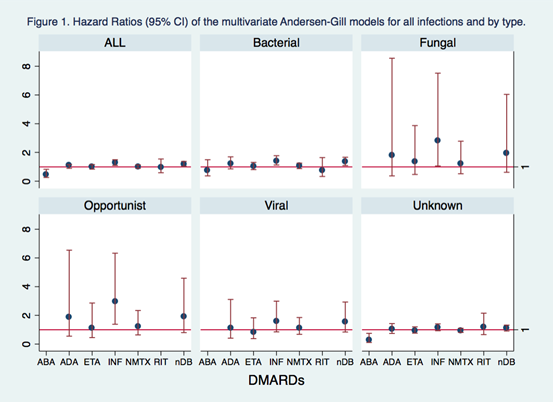
Results: We had 21,727 RA patients participate, with 21% male, a mean (SD) age of 59.0 (13.7) yrs, and 1.7 (1.5) comorbidities. During 92,138 patient-yr follow-up, the treatment exposures included: prednisone (53%), MTX (61%, median 2.4 yrs), NMTX (53%, 1.9 yrs), TNF (50%, 1.5 yrs), and NTNF (8%, 1.4 yrs). There were 2530 serious infections of any type (69 opportunist, 881 bacterial, 114 viral, 43 fungal and 1048 were unable to classify). The most frequent by syndrome were pneumonia (1017), skin (424), and sepsis (367). From the univariate and multivariate analyses, no differences between treatments were found when compared to MTX monotherapy in any group of infections considered. Some exceptions were found: patients who were on INF seemed to be at a higher risk of any infection (HR: 1.29 (1.10-1.50)) and opportunistic infections (2.96 (1.38-6.33)). Patients who took ETA or INF were also at higher risk for skin infections (1.38 (1.04-1.38) and 1.32 (1.00-176), respectively) (Figure 1). When decomposing DMARDs into 5 classes, the results also didn’t change but patients on LEF seemed to be at higher risk for bacterial infections (1.4 (1.12-1.75)), bone/joint (2.01 (1.37- 2.94)) and skin (1.48 (1.11-1.95)). HCQ was protective for pneumonia (0.82 (0.69-0.98)).
Conclusion: Our preliminary results indicated little differences between treatments in risk of serious infections in RA. Next steps will include propensity scores to adjust for possible channeling and to adjust for previous infections and geographical region.
Disclosure:
K. Michaud,
None;
S. Pedro,
None;
A. Kalil,
None;
T. R. Mikuls,
None;
F. Wolfe,
None.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/serious-infection-risk-by-treatments-and-types-in-patients-with-ra/