Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Cognitive symptoms such as forgetfulness or “brain fog” are frequently reported in SLE and among the most distressing symptoms of lupus. Cognitive symptoms are also commonly reported among older adults, but little information is available about cognitive symptoms in older people with SLE compared to those of similar ages with other rheumatic or musculoskeletal conditions. We compared self-reported cognitive function among an older adult cohort with SLE to individuals with rheumatoid arthritis (RA), osteoarthritis (OA), and fibromyalgia (FM) of similar ages, and examined the association of cognitive function with self-perceptions of health status and functioning.
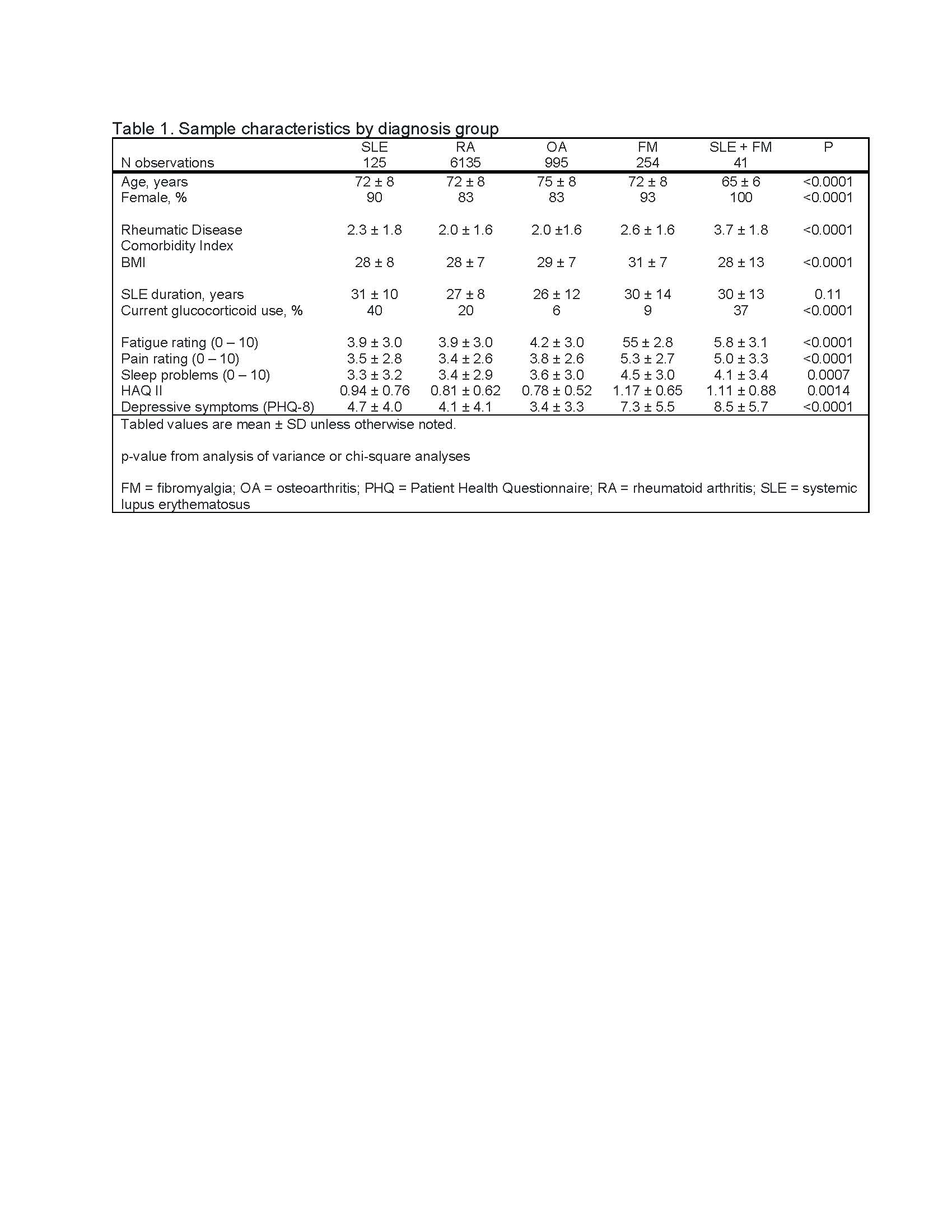
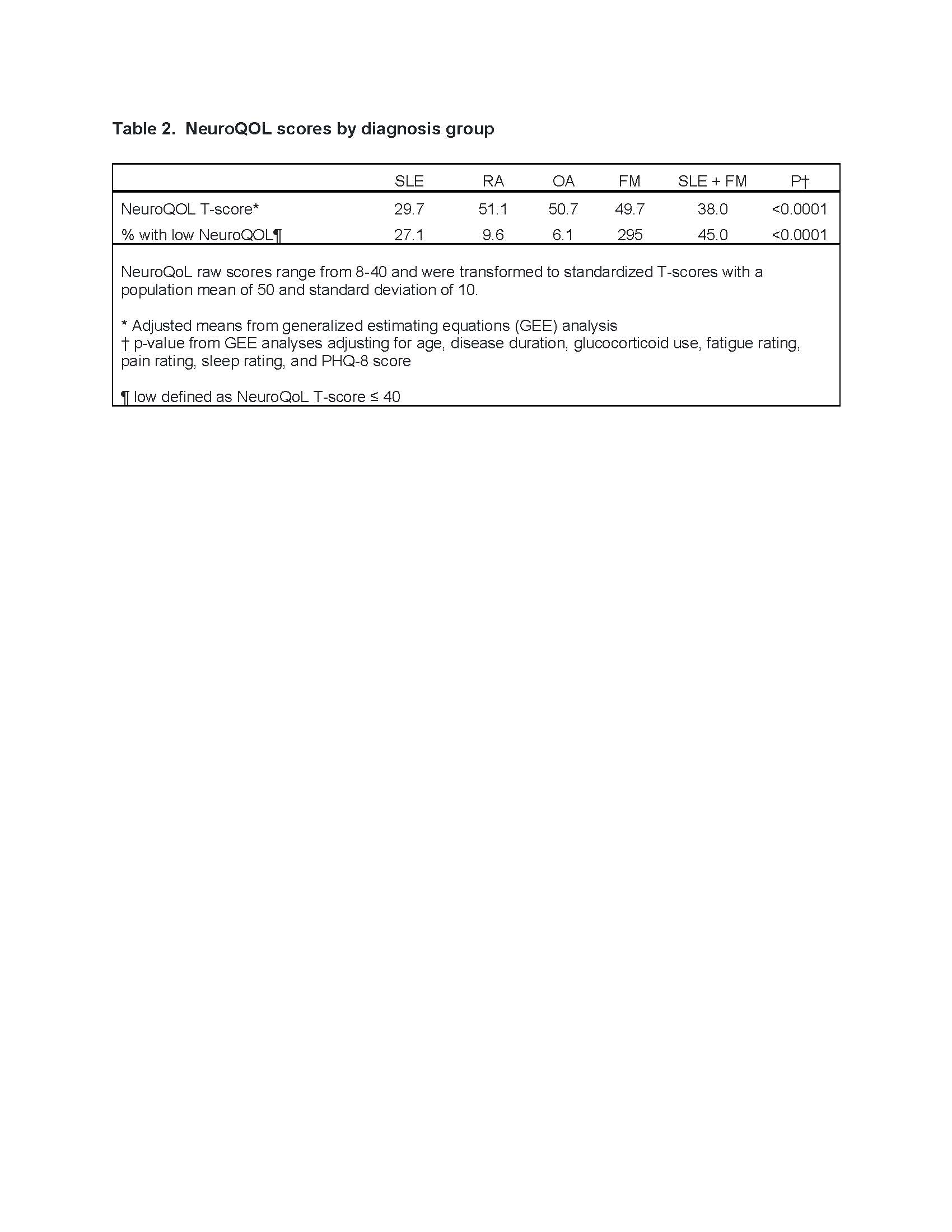
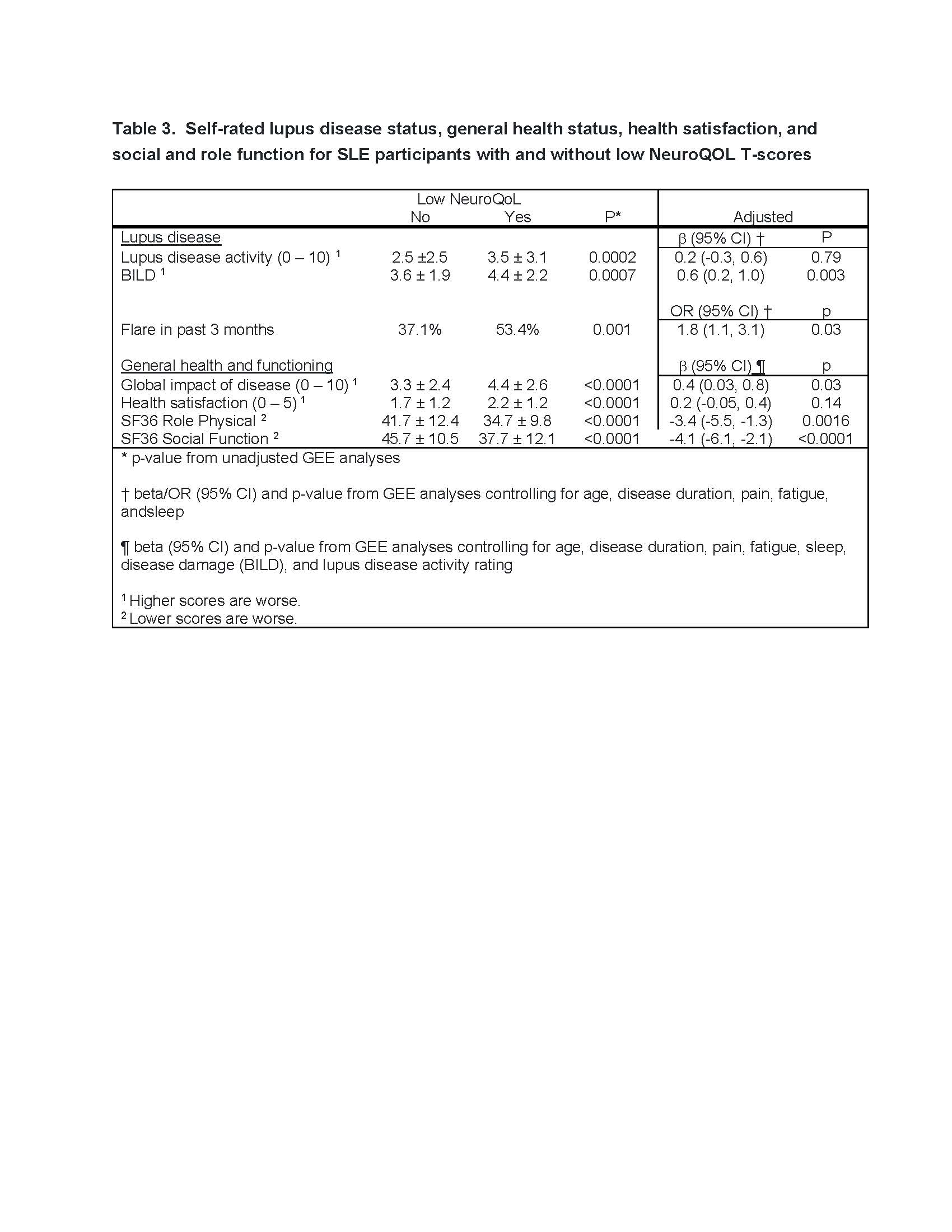
Methods: Data were from FORWARD, The National Databank for Rheumatic Diseases, a longitudinal observational cohort. Data are collected biannually via questionnaires. Individuals with physician-diagnosed SLE, RA, OA, and FM age≥55 were included in analyses. Cognitive symptoms were assessed in 3 biannual surveys with the 8-item NeuroQoL Cognitive Function Short Form (NCF)1, which queries cognitive symptoms and perceived ability to complete everyday tasks. We compared scores of individuals with SLE and no other rheumatic diagnosis to individuals with RA, OA, FM, and SLE + FM using generalized estimating equation (GEE) modeling, adjusting for age, education, pain, fatigue, sleep disturbance, and depressive symptoms. Among the SLE-only group, we compared self-reported lupus disease activity (0-10 scale, 0 = not at all active, 10 = extremely active), organ damage (Brief Index of Lupus Damage, BILD), and the occurrence of flares in the past 3 months between those with low NCF T-scores (below 40, i.e., 1 SD below mean) and those with higher scores. We also compared global health rating (0 – 100), health satisfaction (5-point scale, 0 = very satisfied, 4 = very dissatisfied), and social and role functioning (from SF-36) for those with and without low NCF scores, adjusting for age, education, pain, fatigue, sleep disturbance, depressive symptoms, self-rated lupus activity, and BILD.
Results: 125 SLE, 6135 RA, 995 OA, 254 FM, and 41 SLE+FM questionnaires from respondents ≥ age 55 were completed over 3 periods. Characteristics of each group are shown in Table 1. After adjustment, NCF scores of individuals with SLE alone and SLE +FM were significantly lower than other groups (Table 2). Over a quarter of the SLE group and almost half of the SLE + FM had low NCF scores (Table 2). In the SLE-only group, low NCF scores were associated with significantly higher self-reported disease damage, greater occurrence of flares, and worse global health, health satisfaction, and social and role functioning (Table 3).
Conclusion: Cognitive symptoms are significantly worse among older individuals with SLE compared to individuals of similar age with other rheumatic or musculoskeletal conditions. Results show that the burden of cognitive symptoms continues into older age for individuals with SLE, is significantly greater than for older individuals with other rheumatic/musculoskeletal conditions, and has an important impact on quality of life, above and beyond lupus disease status.
Reference
1Iverson GL et al. Arch Clin Neuropsychol 2021; 36:126-134
To cite this abstract in AMA style:
Katz P, Pedro S, Michaud K. Self-Reported Cognitive Function Among Older Adults with Systemic Lupus Erythematosus (SLE) Compared to Older Adults with Other Rheumatic and Musculoskeletal Conditions [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/self-reported-cognitive-function-among-older-adults-with-systemic-lupus-erythematosus-sle-compared-to-older-adults-with-other-rheumatic-and-musculoskeletal-conditions/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/self-reported-cognitive-function-among-older-adults-with-systemic-lupus-erythematosus-sle-compared-to-older-adults-with-other-rheumatic-and-musculoskeletal-conditions/