Session Information
Date: Sunday, November 5, 2017
Title: Osteoporosis and Metabolic Bone Disease – Clinical Aspects and Pathogenesis Poster I
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: The risk of osteoporotic (OP) fracture among patients with rheumatoid arthritis (RA) is higher than that of the general population. The worldwide incidence of OP fractures in high-risk individuals is expected to double over the next 40 years. It is unknown if improvements in the management of RA and OP has decreased the OP fracture risk in patients with RA. To address this knowledge gap, we compared the risk and incidence of OP fracture among patients with RA to the general population over two chronologic periods.
Methods: Using an electronic medical record database representative of the United Kingdom general population (The Health Improvement Network), we identified patients with incident RA and up to five individuals without RA matched for age, sex, and calendar year of diagnosis between 1999 and 2014. The RA cohort was divided in two sub-cohorts based on the year of RA diagnosis: the early cohort (1999Ð2006) and the late cohort (2007Ð2014). We identified incident OP fracture using physician diagnosis (READ) codes. Subjects with previously-diagnosed prevalent fractures were excluded from this analysis. We calculated the period-specific incidence rates of total OP fracture and hip fragility fracture for each cohort separately. We calculated the hazard ratio (HR) of incident fracture using a Cox proportional hazard model. In the multivariable model, we adjusted for age, body mass index, smoking status (non-smokers, ex-smokers, current smokers), alcohol use (non-drinkers, ex-drinkers, current drinkers), comorbidities, medication use, and the number of PCP visits.
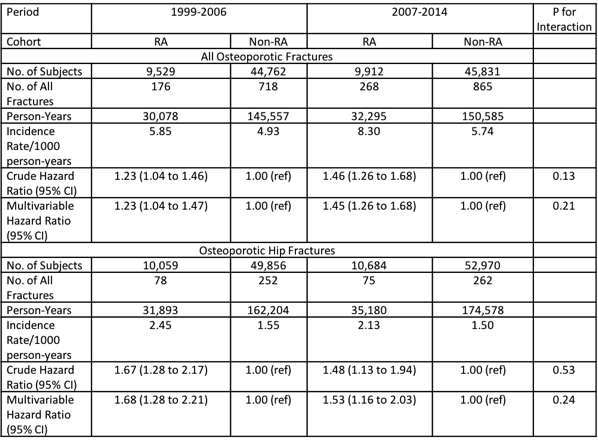
Results: Both the early and late cohorts (N=54,291 and 59,915, respectively) had a similar mean age (60 and 59 years) and sex proportion (~70 and 69% female), and RA patients showed an increased risk of OP fracture compared with their corresponding comparison cohort (Table). In both cohorts, the incidence rate of total OP fracture slightly increased, and the corresponding relative risk (RR) was not significantly different between the two periods (corresponding multivariable HRs=1.23 [95% CI: 1.04 to 1.47] vs. 1.45 [95% CI: 1.26 to 1.68]; p for interaction = 0.21) (Table). Meanwhile, in both cohorts, the incidence rate of hip fragility fracture slightly declined and the corresponding RR was not significantly different between the two periods (corresponding multivariable HRs=1.68 [95% CI: 1.28 to 2.21] and 1.53 [95% CI: 1.16 to 2.03]; p for interaction = 0.24) (Table).
Conclusion: This general population-based cohort study indicates that RA patients still experience a higher risk of all OP and hip fragility fractures compared to non-RA patients, and that this difference has not improved over the past several decades despite advances in RA and OP therapy. This unclosing gap in increased fracture risk among RA patients calls for improved management of osteoporosis in RA.
To cite this abstract in AMA style:
Keller S, Bolster MB, Oza A, Rai SK, Lu L, Zhang Y, Choi HK. Secular Trends in the Risk of Fragility Fracture Among Patients with Rheumatoid Arthritis: A General Population-Based Study [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/secular-trends-in-the-risk-of-fragility-fracture-among-patients-with-rheumatoid-arthritis-a-general-population-based-study/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/secular-trends-in-the-risk-of-fragility-fracture-among-patients-with-rheumatoid-arthritis-a-general-population-based-study/