Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Ultra violet light (UV) exposure has been implicated as a major contributor to pathogenesis and flares in lupus. While some studies have looked at the association between seasons (as proxy for sun exposure) and cutaneous or systemic flares in lupus patients, results are mixed and few include racially diverse cohorts. Our objectives were to study whether a seasonal relationship exists with cutaneous and systemic lupus flares in a racially and ethnically diverse cohort of pediatric and adult lupus patients.
Methods: We retrospectively analyzed consecutive study visits from 2002-2019 of adult and pediatric lupus patients enrolled in the Einstein Lupus Cohort at Montefiore Medical Center in Bronx, NY. We defined cutaneous flare by SELENA SLEDAI inflammatory rash, and systemic flare as SLEDAI ≥ 4. Mixed-effects regression models were used to determine whether cutaneous or systemic flares were associated with season adjusting for race/ethnicity and sex as potential confounders and accounting for repeated measures for each patient. We examined the relationship in a second model including average UV index (UVI) in New York City for the month preceding study visits, to account for the expected lag between UV exposure and onset of symptoms.
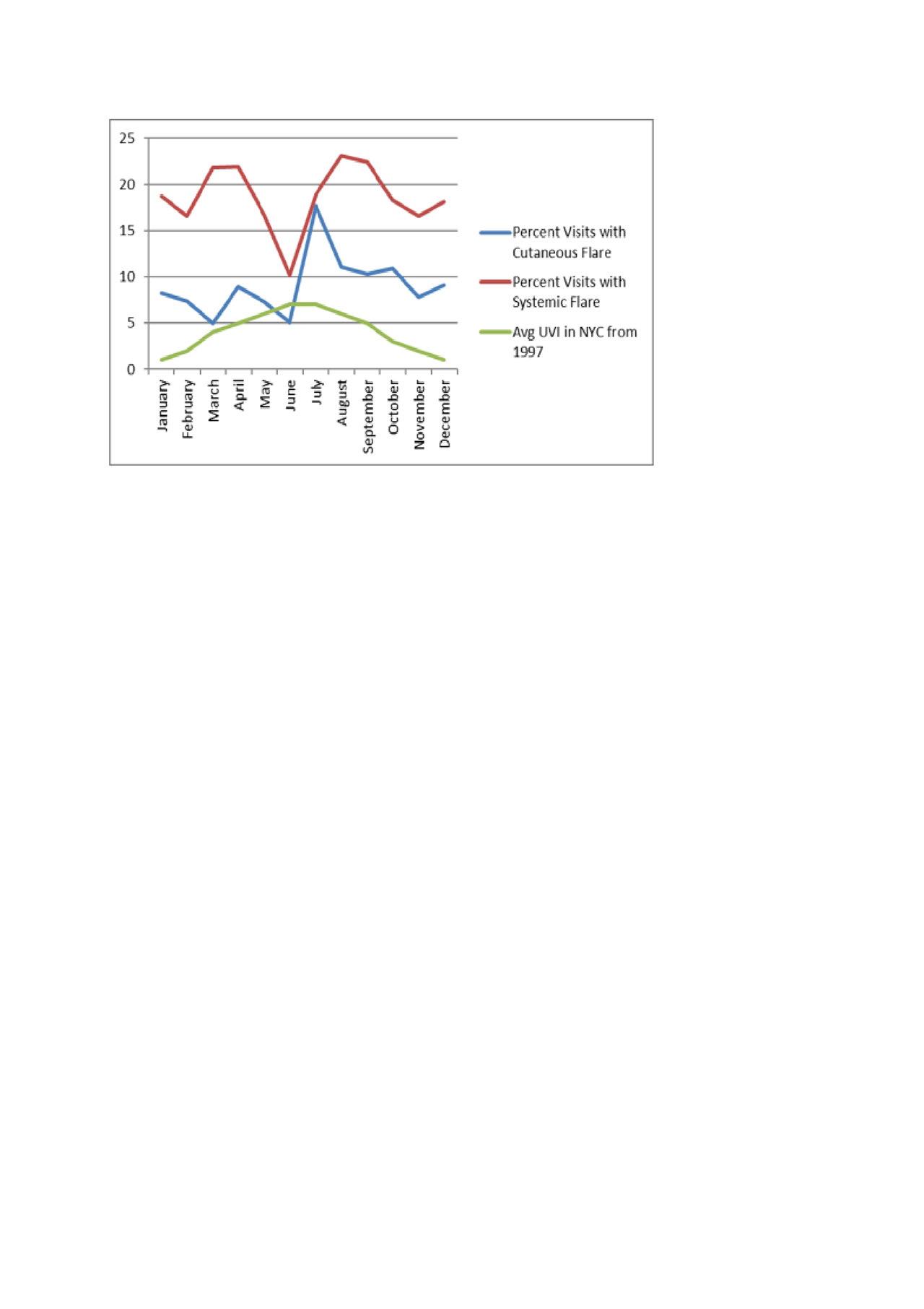
Results: We examined 2,351 patient visits for 704 individual patients. Our patients were 87% female; 36% were Black non-Hispanic, 47% were Hispanic and 3% were white non-Hispanic. Among all visits, 9% were associated with new inflammatory rash. Looking at cutaneous disease in a mixed effects model, to account for repeated measures from the same patient, we found that summer (July-Sept) was significantly associated with cutaneous flare compared to winter (Jan-Mar); results remained significant when we adjusted for race/ethnicity and sex (OR 1.8, [95% CI 1.0-3.1], p=0.04). Once adjusting for the previous month’s UVI there was no longer an association between summer and cutaneous flare. There was no association between season and systemic flare (OR 1.0 [95% CI 0.7-1.4], p=0.9). However, a bi-modal distribution of systemic flare rates was observed (1st peak in Mar/April, 2nd peak in July-Oct). In an adjusted mixed-effect model with sex, race/ethnicity and previous month’s UVI included, Mar/April and Jul-Oct were both still significantly associated with systemic flare compared to other months: Mar/April (OR 2.0 [95% CI 1.4-2.9], p< 0.001), Jul-Oct (OR 2.9 [95% CI 1.7-4.7], p< 0.001).
Conclusion: We found as association between cutaneous flare and summer in a racially and ethnically diverse cohort of patients with SLE, a relationship that appears to be mostly explained by the previous month’s UVI. Though we found no association between systemic flare and season, a bimodal relationship was observed in systemic flares with peak rates in early spring and again in summer through early fall. These two peak periods were associated with systemic activity even while accounting for previous month’s UVI. Further epidemiologic studies examining other potential exposures that vary with season may help elucidate triggers that help explain this relationship.
To cite this abstract in AMA style:
Tanner T, Wahezi D, Agalliu I, Putterman C, Broder A, Jordan N, Maldonado Andujar D, Rubinstein T. Seasonality of Cutaneous and Systemic Flares in Adults and Children in the Einstein Lupus Cohort [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/seasonality-of-cutaneous-and-systemic-flares-in-adults-and-children-in-the-einstein-lupus-cohort/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/seasonality-of-cutaneous-and-systemic-flares-in-adults-and-children-in-the-einstein-lupus-cohort/