Session Information
Session Type: Poster Session C
Session Time: 1:00PM-3:00PM
Background/Purpose: While the seasonal variation of systemic lupus erythematosus (SLE) disease activity has been reported, population-based studies are still lacking. Here we investigate the seasonal variations of hospitalizations and in-hospital mortality related to SLE using a US-based national database.
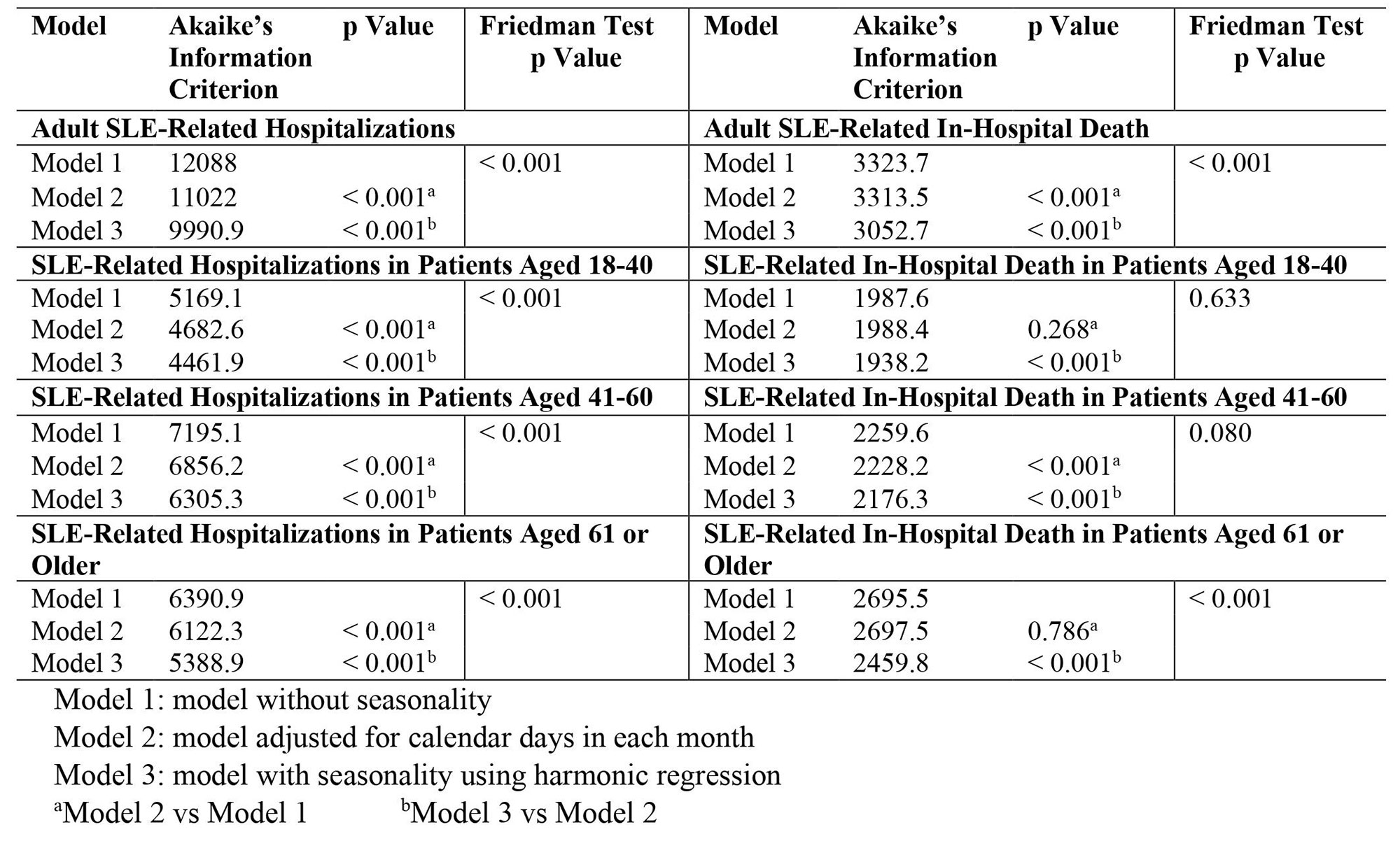
Methods: We examined adult SLE-related hospitalizations using Nationwide Inpatient Sample (NIS) from 2005 to 2019. Records of SLE-related hospitalizations were identified with ICD-9 code 710.0 and ICD-10 code M32. Weight-adjusted monthly hospitalizations and in-hospital death were used for analysis. In this study, we utilized two methods to examine the seasonality of SLE-related hospitalizations and in-hospital mortality. First, we conducted Poisson regression analysis to explore the trend of SLE-related hospitalization and in-hospital mortality over time (model 1 and model 2). Fourier series were later added to fit the seasonality component (model 3). Akaike’s Information Criterion (AIC) and analysis of variance (ANOVA) were used to compare the models and detect seasonality. Then, we performed Friedman test on detrended data to confirm the presence of seasonality. Finally, we analyzed the peak and trough of SLE-related hospitalization and in-hospital death among different age groups if seasonality was present using both methods. p < 0.05 was considered statistically significant. All statistical analyses were conducted using R Statistical Software, version 4.1.2 (R Foundation for Statistical Computing, Vienna, Austria).
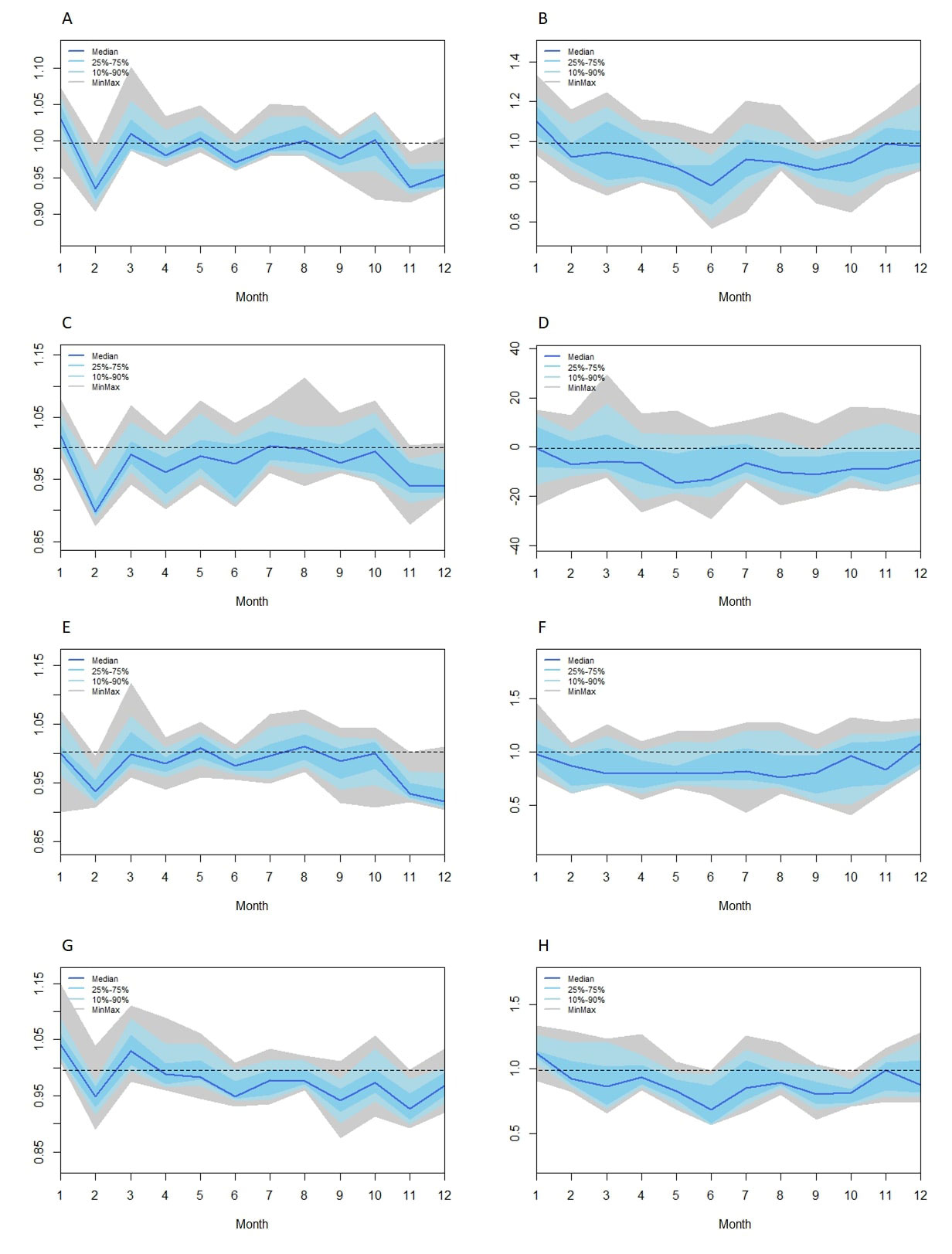
Results: SLE-related hospitalizations increased, and SLE-related in-hospital mortality decreased over the study period. There was seasonal variation in the hospitalization and in-hospital death in adult SLE patients (Table 1). Among all adult patients, SLE-related hospitalizations were highest in January and lowest in February. SLE-related in-hospital mortality was highest in January and lowest in June. In patients aged between 18 and 40 years old, SLE-related hospitalizations were highest in January and lowest in February. In patients aged between 41 and 60 years old, SLE-related hospitalizations were highest in August and lowest in December. In patients aged 61 years or older, SLE-related hospitalizations were highest in January and lowest in February. SLE-related in-hospital mortality was highest in January and lowest in June (Figure 1).
Conclusion: There was an increase in the number of SLE-related hospitalizations and a decrease in SLE-related in-hospital mortality from 2005 to 2019. A significant seasonal component in SLE-related hospitalizations and in-hospital deaths was observed, although the patterns of seasonality varied among different age groups.
To cite this abstract in AMA style:
Zheng J, Ni R, Zou G, Xi Q, Hsieh T, Abdollahi S. Seasonal Variation of Hospitalizations and In-Hospital Mortality Related to Systemic Lupus Erythematosus Among Adults in the United States: An Analysis of Nationwide Inpatient Sample [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/seasonal-variation-of-hospitalizations-and-in-hospital-mortality-related-to-systemic-lupus-erythematosus-among-adults-in-the-united-states-an-analysis-of-nationwide-inpatient-sample/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/seasonal-variation-of-hospitalizations-and-in-hospital-mortality-related-to-systemic-lupus-erythematosus-among-adults-in-the-united-states-an-analysis-of-nationwide-inpatient-sample/