Session Information
Date: Sunday, October 21, 2018
Title: Pediatric Rheumatology – Clinical Poster I: Lupus, Sjögren’s Disease, and Myositis
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Exposure to sunlight has been proposed as a possible environmental trigger for lupus flares, particularly cutaneous disease. Contradictory findings exist regarding seasonal variation in cutaneous disease activity, with particular gaps in knowledge around pediatric and minority patient populations.
Our objectives for this study were to study the relationship between sun exposure and cutaneous lupus flares in a racially and ethnically diverse pediatric lupus population. Based on prior studies, we hypothesized that higher rates of cutaneous flares would be present in summer/fall compared to winter/spring seasons.
Methods: We retrospectively reviewed 12 years of data from patients enrolled in the Pediatric Einstein Lupus Cohort at the Children’s Hospital at Montefiore from the Bronx, New York. We selected patients that had any history of mucocutaneous disease by indicated by BILAG scores of A-D, as opposed to E, at any point during follow up. We defined cutaneous flares by two methods: (1) mucocutaneous BILAG criteria A or B and (2) SLEDAI-2K inflammatory rash criteria. Chi-square tests were used to compare flare rates during summer/fall vs winter/spring and to compare flare rates during each season.
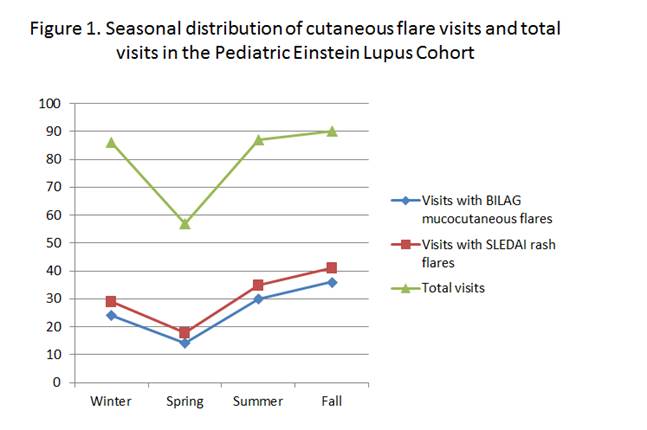
Results: We examined 320 visits for 90 individual patients. The average age of participants at included visits was 16.8 ±3 years; 82% of patients were female; 52% were Hispanic and 43% Black. Among included visits, 33% had represented BILAG-mucocutaneous flares and 38% represented SLEDAI-rash flares. Total visits and flare visits were not evenly distributed throughout the year; more total visits and more flare visits were observed during summer/fall (Figure 1). The rate of visits with BILAG-mucocutaneous flares was 37% in the summer/fall vs 27% in winter/spring (p = 0.04). The rate of visits with SLEDAI-rash flares was 43% in summer/fall vs 33% in winter/spring (p = 0.05) (Table 1). In contrast, there was no significant association between specific seasons and BILAG-mucocutaneous flares or SLEDAI-rash flares, though the highest flare rates were observed during fall (40%, 46% of visits, respectively).
Conclusion: Our results show a modestly increased rate of cutaneous flares during summer/fall months when compared with winter/spring months in a racially and ethnically diverse sample of children with SLE. More studies are needed to better understand the relationship between sun exposure and disease flare in minority race/ethnicities with pediatric lupus to inform disease activity prevention counseling.
|
Table 1. Rates of cutaneous flare in pediatric lupus patients |
|||
|
|
Summer/Fall visits (N = 177) |
Winter/Spring visits (N = 143) |
p value: |
|
Mucocutaneous flare visits by BILAG |
66 (37%) |
38 (27%) |
0.04 |
|
Inflammatory rash flare by SLEDAI |
76 (43%) |
47 (33%) |
0.05 |
To cite this abstract in AMA style:
Tanner T, Dionizovik-Dimanovski M, Wahezi D, Rubinstein T. Seasonal Variation in Cutaneous Flares for Pediatric Lupus [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/seasonal-variation-in-cutaneous-flares-for-pediatric-lupus/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/seasonal-variation-in-cutaneous-flares-for-pediatric-lupus/