Session Information
Date: Tuesday, November 14, 2023
Title: (1996–2018) Osteoporosis & Metabolic Bone Disease – Basic & Clinical Science Poster
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
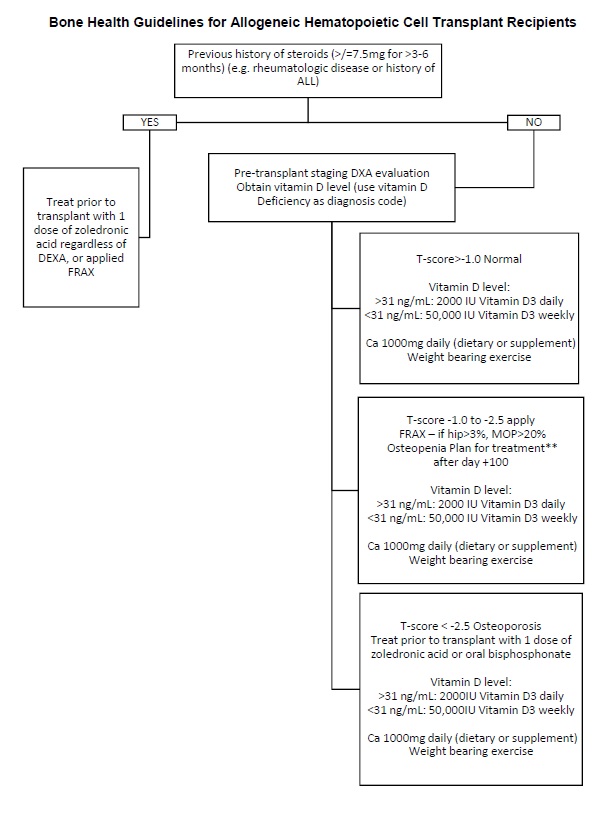
Background/Purpose: Bone mineral density (BMD) loss and fracture are important causes of increased morbidity following allogeneic hematopoietic stem cell transplant (allo-HCT).Recent societal recommendations support screeningDual X-ray Absorptiometry (DXA) both before and within 1 year after allo-HCT. Our institutionimplemented a new management algorithm that emphasized pre-transplant screening for allo-HCT patients and contained guidance on use of bone strengthening agentstoimproveBMDrelated outcomes in this population. This study evaluatedthe rate of screening and treatment of low BMD and fracture in allo-HCT patients and determined the effect that the quality improvement intervention had on these measures.
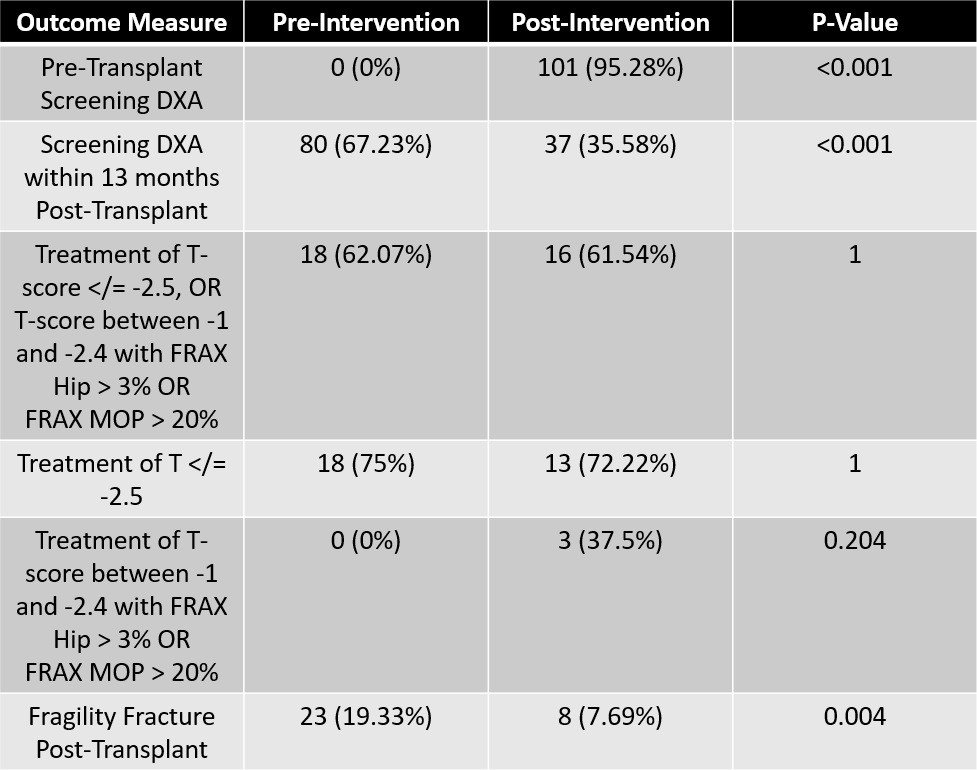
Methods: This was a retrospective chart review ofallo-HCT recipients at the Cleveland Clinic Foundationfrom April 2016 toMarch 2022. 244 patients with at least 1-year of follow up from allo-HCT were identified for analysis.The BMD management algorithm was implemented in 10/2019, and we compared rates of DXA screen (pre- and post-HCT), treatment, and fragility fractures between allo-HCT recipients before and after this time point.We also analyzed available T-scores at the spine, femoral neck, and total hip and FRAX risk scores before and after allo-HCT. Treatment was guided by National Osteoporosis Foundation (NOF) recommendations (T-score of −2.5 or less, or T-score of –1 to –2.4 and a 10-year probability of hip fracture >/= 3% or any major fracture >/= 20% as calculated by FRAX).
Results: After intervention, thepre-transplant DXA screening increased from 0% to 95%, though post-transplant DXA screening (≤13 months from HCT) decreased from 67% to 36% (p < 0.001). Rate of treatment indecreased from 67.23%to 35.58% (p < 0.001).Rate of treatment in patients meeting NOF criteria was similar pre- and post-intervention (62% vs 62%). Subgroup analysis showed treatment of osteoporosisalso remained similar between groups (75% vs 72%),however the rate of treatment of osteopenia with a high FRAX score was improved in the post-intervention group (0% vs 38%, p = 0.204). The fracture rate was significantly lower in the post-intervention group (7.7% vs 19.3%, p = 0.004).
Conclusion: Implementation of analgorithm for screening and treatment of low BMD in allo-HCT recipientswith a focus on pre-transplant DXA screening resulted in an expected increase in pre-transplant screening, but anunexpected decreased rate of follow-up DXA within the 13 months post-transplant. This intervention alsoledto an increased rate of treatment of patients with osteopenia and elevated FRAX. The intervention led to a significantly decreased rate of fractures, which may be related to the increased awareness of low BMD and potentially due to the timing of treatment initiation, which was not directly assessed in this analysis.Allo-HCT patients are a complex population of patients that are prone to low BMD and focusing on the detection and management of this important cause of morbidity is correlated with improved outcomes.
To cite this abstract in AMA style:
Fuchs P, Ferraro C, Zhang C, Deal C, Hamilton B, Keller S. Screening and Treatment of Low Bone Mineral Density in Allogeneic Hematopoietic Cell Transplant Patients [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/screening-and-treatment-of-low-bone-mineral-density-in-allogeneic-hematopoietic-cell-transplant-patients/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/screening-and-treatment-of-low-bone-mineral-density-in-allogeneic-hematopoietic-cell-transplant-patients/