Session Information
Title: Systemic Sclerosis, Fibrosing Syndromes, and Raynaud’s - Clinical Aspects and Therapeutics II
Session Type: Abstract Submissions (ACR)
Background/Purpose: Systemic sclerosis (SSc) commonly leads to pulmonary hypertension (PH), which may be associated with left heart disease and an elevated pulmonary capillary wedge pressure (PCWP). Patients in this PH subgroup may have pulmonary artery pressures (PAP) in proportion to their elevated PCWP (pulmonary venous hypertension, “PVH”) or higher than expected given their PCWP (“out-of-proportion PH”). It is not known what causes this difference in patients with SSc.
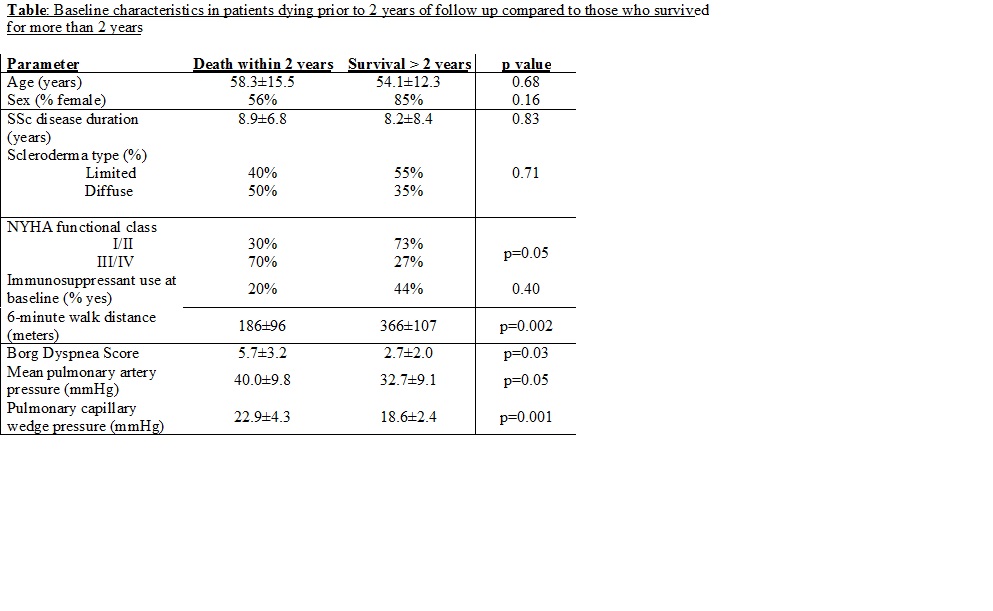
Methods: Baseline characteristics from 48 patients in the PHAROS registry (a prospective observational cohort of SSc patients at high risk for or with PH) who had a PCWP>15 on their inclusion right heart catheterization (RHC) were retrospectively analyzed. Using unpaired t-tests, characteristics of those who died before 2 years of follow-up (n=10) were compared to those who were alive at 2 years (n=20). Patients were divided into 2 groups based on their initial RHC diastolic pressure gradient (DPG=diastolic PAP minus PCWP): PVH (DPG ≤5mmHg) or out-of-proportion PH (DPG˃5mmHg). Comparisons were made between groups using unpaired t-tests or Chi square. Kaplan-Meier analysis compared survival and time to first hospitalization between the 2 groups.
Results: At baseline, the mean PAP (mPAP) was 36.8±11.8 mmHg and the PCWP was 19.4±3.3mmHg. Univariate factors associated with death prior to 2 years are shown in the table. In multivariate analysis, the only independent factors associated with death prior to 2 years were lower 6MWD (p=0.01) and higher PCWP (p= 0.01). The out-of-proportion PH group (n=26) had higher baseline mPAP (42.7±13.0 vs. 29.7±3.7mmHg, p<0.0001), DPG (12.7±8.6 vs. 2.9±1.5mmHg, p<0.0001), and pulmonary vascular resistance (376±235 vs. 204±101 dynes/sec/cm5, p=0.003) compared to the PVH group (n=22). Although there was no difference in baseline immunosuppression use overall, mycophenolate use was less common in the out-of-proportion PH group (8% vs. 37%, OR 0.15, p=0.027). There were no differences between the PVH and the out-of-proportion PH groups in age, sex, disease duration, pulmonary function, SSc subtype, or 6MWD (all p>0.05). There was no difference in 3-year survival between the 2 subgroups (PVH: 1-year=95%, 3-year=61%; out-of-proportion PH: 1-year=85%, 3-year=63%, p=0.73). There was a trend towards a shorter time to first hospitalization in the out-of-proportion PH group (p=0.13).
Conclusion: In patients with SSc-PH and a PCWP>15, lower 6MWD and higher PCWP were independently associated with an increased risk for death within 2 years. In SSc patients with a PCWP>15, those with out-of-proportion PH were less likely to be on mycophenolate (MMF) compared to those with pulmonary venous hypertension. The relationship between MMF and PH in SSc needs further investigation, as MMF’s anti-fibrotic effects may theoretically decrease pulmonary artery remodeling in these patients.
Disclosure:
M. R. Lammi,
None;
L. A. Saketkoo,
Gilead Pharmaceuticals,
2,
United Therapeutics,
2,
Actelion Pharmaceuticals US,
2;
J. K. Gordon,
None;
P. Lauto,
None;
V. D. Steen,
Gilead Science, ,
2,
Gilead Science,
5,
Actelion Pharmaceuticals US,
2,
Actelion Pharmaceuticals US,
8,
Roche Pharmaceuticals,
2,
Celgene,
2,
Sanofi-Aventis Pharmaceutical,
2.
« Back to 2013 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/scleroderma-patients-with-pulmonary-hypertension-and-increased-pulmonary-capillary-wedge-pressure-in-the-pulmonary-hypertension-assessment-and-recognition-of-outcomes-in-scleroderma-pharos-cohort/