Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Ophthalmologists increasingly call rheumatologists for the evaluation and treatment of scleritis. Although they can be of immune etiology (systemic or restricted to the eye), infectious causes are also possible, and sometimes recognizing them is a diagnostic challenge. Although the reasoning behind comparing uveitis and the affected eye segment is well established, little is known about whether a similar strategy can be used in the approach to scleritis.
Methods: This single-center, cross-sectional study evaluated all patients diagnosed with scleritis at a center specializing in rheumatology and ophthalmology. The diagnosis of scleritis was established on the basis of ophthalmological diagnosis, as well as its classification as non-specific anterior scleritis, posterior scleritis, diffuse anterior scleritis, anterior nodular scleritis, necrotizing anterior scleritis, and sclero-uveitis. Patients were divided and compared according to the following criteria: immune scleritis (immune-mediated scleritis of systemic etiology or immune-mediated scleritis restricted to the eye) or infectious scleritis.
This categorization was based on an analysis of the medical records. Immune-mediated scleritis restricted to the eye was considered in patients whose rheumatological investigation did not define a systemic cause and whose infectious investigation was negative. Descriptive epidemiology, Fisher, and chi-square tests were used for statistical analysis. The R4.3.2 software was used for the statistical analyses.
Results: Between January 2023 and April 2024, 53 patients were selected as having a diagnosed with scleritis. The average age was 50,6+- 15 years-old and the predominant sex was female. Of these, 25 (48%) corresponded to systemic etiology, the main ones being RA, GPA, and RP. 21 (40,3%) patients were classified as having an immune etiology restricted to the eye and 6 (11,5%) as having infectious causes. Among the infectious causes, these were the etiologies: Bartonella sp, Pseudomonas sp, post Herpetica, Syphilis and Tuberculosis.
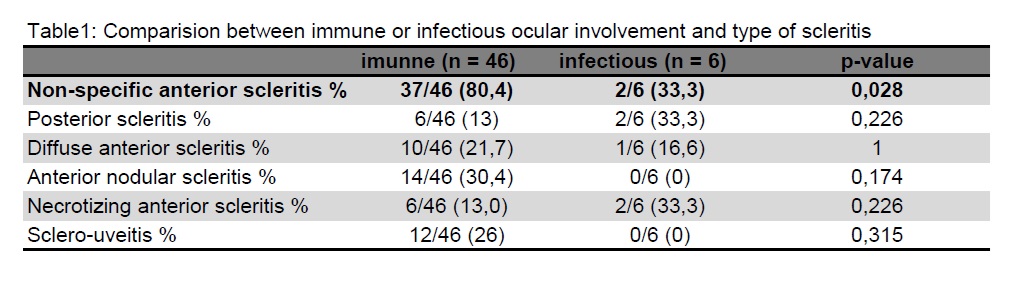
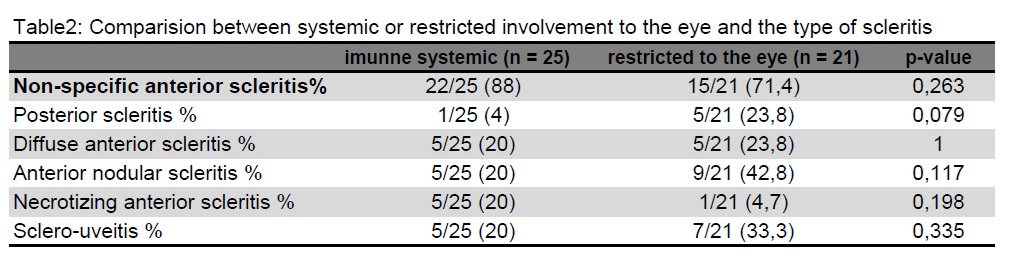
When comparing immune causes (systemic and restricted to the eye) with infectious causes, there were more patients with immune etiologies affecting the anterior sclera than infectious causes (80,4% vs 33,3% p: 0,028) (Table 1). When comparing immune causes, there was no difference in the type of scleritis that indicated a systemic or eye-restricted cause (Table 2).
Conclusion: In our sample, infectious causes of scleritis were in the minority (and differed from immune causes by having little preference for the anterior sclera). The type of scleritis does not seem to help distinguish a systemic cause from an immune-mediated etiology restricted to the eye, and the latter should only be considered after an extensive investigation.
To cite this abstract in AMA style:
Caroline Antunes Dos Santos H, Sachetto Z, da rocha jorge R, Vilaça Gutierrez G, Froes Ramos de lima R, Ribeiro Fretes A, zacarin M, dos reis R, Pugliesi A. Scleritis and the Rheumatologist. Does the Type of Scleritis Help to Distinguish an Infectious Cause from an Immune Cause? Among the Immune Causes, Does It Help Differentiate Between Systemic Causes and Those Limited to the Eye? [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/scleritis-and-the-rheumatologist-does-the-type-of-scleritis-help-to-distinguish-an-infectious-cause-from-an-immune-cause-among-the-immune-causes-does-it-help-differentiate-between-systemic-causes-a/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/scleritis-and-the-rheumatologist-does-the-type-of-scleritis-help-to-distinguish-an-infectious-cause-from-an-immune-cause-among-the-immune-causes-does-it-help-differentiate-between-systemic-causes-a/