Session Information
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: It has been hypothesized that autoimmunity may play a role in the pathophysiology of schizophrenia (SCZ). Several autoimmune disorders (AID) have also been noted to be prevalent in schizophrenics.. We aim to record the prevalence of different AID in schizophrenia patients, and determine clinical characteristics and inpatient outcomes for this patient population.
Methods: We obtained data from National Inpatient Sample (NIS), which was further optimized to national estimates. Hospitalizations with principal diagnosis of Schizophrenia with and without a pre-existing AID in patients above 18 years was taken from the 2016-2018 database. The AIDs included were Type 1 diabetes mellitus (DM), Rheumatoid arthritis (RA), Systemic Lupus Erythematosus (SLE), Multiple Sclerosis (MS), Autoimmune thyroid disease (ATD), Myasthenia Gravis (MG), ANCA associated vasculitis (AAV), Systemic sclerosis (SSc), Dermato-polymyositis (DPM), Giant cell arteritis with Polymyalgia Rheumatica (GCA-PMR), Sjogren Syndrome (SS) and Celiac disease (CD). Multivariate logistic regression model was used to calculate the adjusted odds ratio for SCZ and SCZ-AID. Epidemiological differences and outcomes of length of stay (LOS), mortality, and total hospital charges (THC) were compared. Multivariable logistic and linear regression analyses were used to adjust for confounding variables.
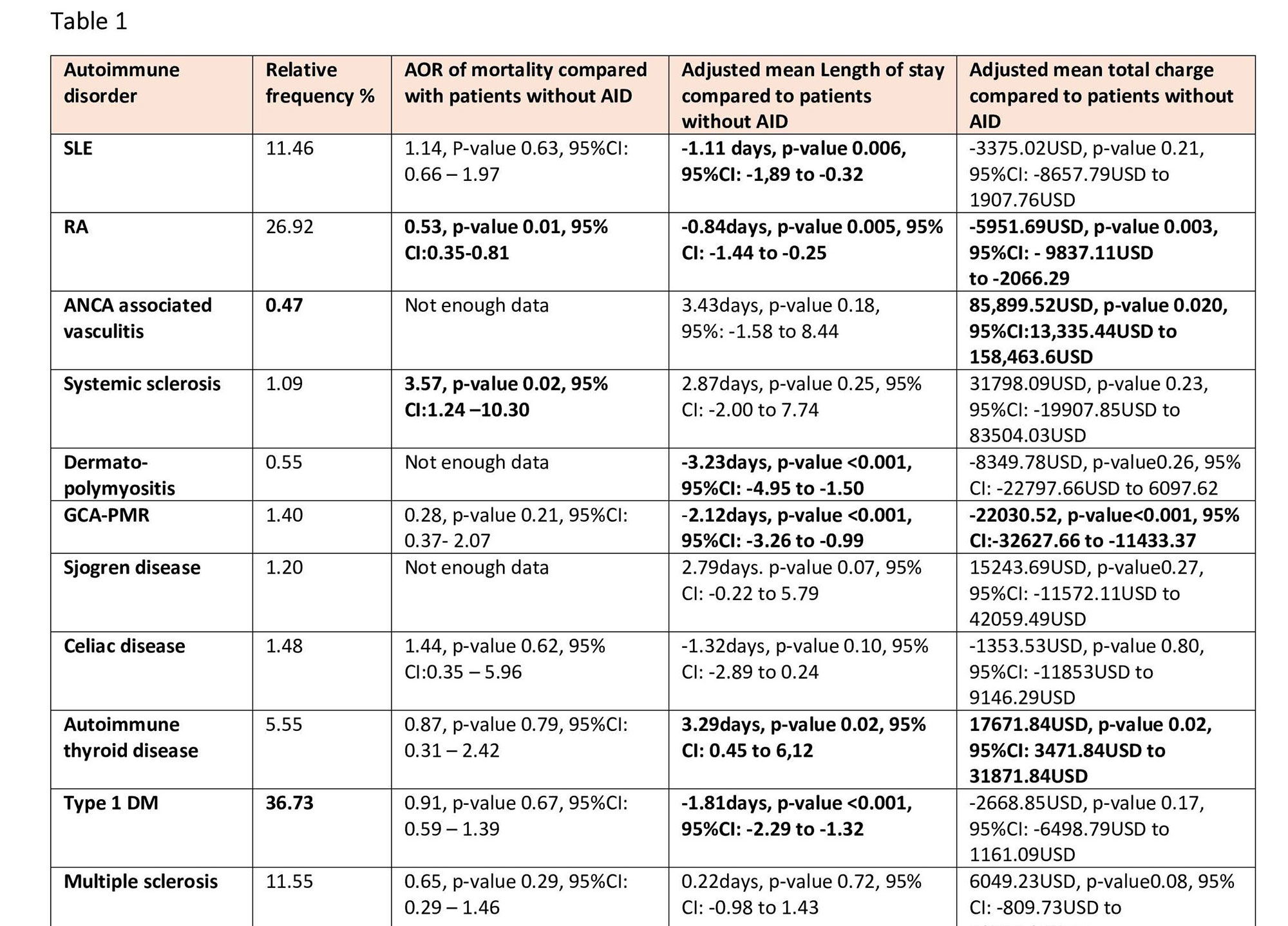
Results: A total number of 1,220979 hospitalizations with principal diagnosis SCZ were identified between 2016 -2018. Among these, 2.63 % patients had at least one AID. Patients with SCZ and SCZ-AID had mean ages of 50.7 and 50.3 years, respectively. Among SCZ-AID patients, 56.8% were females, compared to 38.7% females in SCZ alone. SCZ-AID population was predominantly white (51.28%), and 0.59% were Native Americans. Most prevalent AIDs were DM (36.3%), RA (26.92%), SLE (11.46%), and MS (11.44%). Schizophrenics with AID spent at least 0.84 days less in hospital with an adjusted mean difference of -0.48 days (CI: -1.20–0.48, p< 0.001). Mortality rate in patients with SCZ SCZ-AID was 1.42% and 1.23% respectively (OR: -0.74, CI: 0.59 – 0.94, p=0.014). SCZ-AID patients had 26% less odds of in-hospital mortality from all causes. The highest death rate was among AAV (5.7%) and the least among DM patients (0.095%). There was no significant difference in total hospital charge (p=0.58). In subgroups, the highest total charge occurred among ANCA vasculitis and least among GCA-PMR patients.
Conclusion: AID is common among in-patients with schizophrenia, with type 1 diabetes mellitus, SLE and RA being the top 3 AID diagnosis. Females had 2-fold odds of having associated AID diagnosis. The coexistence of AID in patients with schizophrenia was associated with lower all cause in-patients’ deaths and shorter LOS. These outcomes most likely may be related to the relatively younger and predominantly female population with AID compared to cohort making the likelihood of being admitted with more advance and potentially fatal diseases less. This hypothesis may need prospective studies to ascertain in other to guide clinical decision making.
To cite this abstract in AMA style:
Sami F, Kumi D, Liaqat S, Sami H. Schizophrenia and Its Relationship with Autoimmunity: A Nationwide Analysis [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/schizophrenia-and-its-relationship-with-autoimmunity-a-nationwide-analysis/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/schizophrenia-and-its-relationship-with-autoimmunity-a-nationwide-analysis/