Session Information
Date: Tuesday, November 9, 2021
Title: Patient Outcomes, Preferences, & Attitudes Poster IV: COVID-19 (1589–1613)
Session Type: Poster Session D
Session Time: 8:30AM-10:30AM
Background/Purpose: Whether patients with chronic rheumatic diseases (CIRD) are at increased risk of developing severe COVID 19 infections is not entirely clear. However, some DMARDs seem to be associated with worse outcomes. Out of this perspective vaccination protection should be sought for all CIRD patients. Recent surveys showed in CIRD patients an alarming degree of vaccine hesitancy1. Strategies should be developed to increase the vaccination rates in patients with CIRD.
To identify sociodemographic, patient and disease specific predictors of vaccine willingness in CIRD patients and to compare these with a control group.
Methods: Using a cross-sectional study design, a survey was conducted to assess vaccination willingness of consecutive CIRD patients and controls without CIRD presenting to our tertiary rheumatology hospital. In addition to sociodemographic data, patient and disease characteristics including comorbidities and therapy were recorded. A numerical rating scale was used to measure vaccination willingness (0: fully disagree; 10: fully agree). Definite willingness to be vaccinated was assumed if ³7 was selected. Nonparametric tests and multivariate linear regression were performed where appropriate.
Results: A total of 514 CIRD patients and 100 controls were prospectively included (table 1). No significant differences were found regarding the definite vaccination willingness (79.6% vs. 76%) in CIRD vs. control patients. In the CIRD group, the willingness to be vaccinated against SARS-CoV-2 showed a moderate positive correlation with the level of information on influenza and pneumococci as well as a history of travel vaccination (table 2); this was not the case in the control group.
Furthermore, a positive correlation was found in CIRD patients with age and an even stronger with educational level, but no correlation was seen with known risk factors for severe outcomes of COVID-19 disease except for hypertension. A status of “no comorbidity” was associated with a lower vaccine acceptancy in CIRD patients. Finally, neither the number nor the type of current immunosuppressive therapy correlated with vaccination willingness. CIRD patients, who did not think that they are at risk for a COVID 19 disease were less likely to accept a SARS-CoV-2 vaccination.
Conclusion: The majority of CIRD patients was ready to be vaccinated against SARS-CoV-2. This was especially the case in older patients, those with a higher educational level and those who rated themselves as being at increased risk. Moreover, our survey highlights several factors that are relevant for vaccination willingness, including appropriate information about preventable infections and its relevance in general. The fact that known risk factors for a severe COVID-19 did not show an interference with vaccine acceptancy is alarming and indicates that more patient education is needed.
Reference:
1. Felten R et al. Vaccination against COVID-19: Expectations and concerns of patients with autoimmune and rheumatic diseases. Lancet Rheumatol 2021
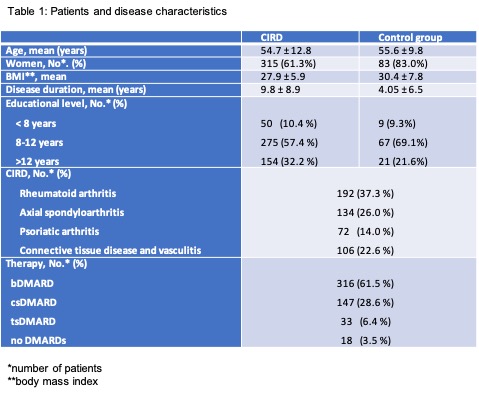 Table 1: Patients and disease characteristics
Table 1: Patients and disease characteristics
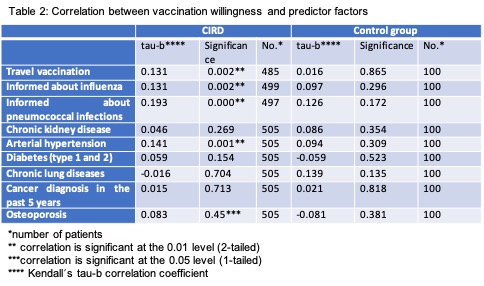 Table 2: Correlation between vaccination willingness and predictor factors
Table 2: Correlation between vaccination willingness and predictor factors
 Figure 1: Vaccination willingness of CIRD patients
Figure 1: Vaccination willingness of CIRD patients
To cite this abstract in AMA style:
Roman I, Andreica I, Baraliakos X, Kiltz U, Braun J. SARS-CoV-2 Vaccination Willingness and Its Predictors in Patients with Chronic Inflammatory Rheumatic Diseases (CIRD) [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/sars-cov-2-vaccination-willingness-and-its-predictors-in-patients-with-chronic-inflammatory-rheumatic-diseases-cird/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/sars-cov-2-vaccination-willingness-and-its-predictors-in-patients-with-chronic-inflammatory-rheumatic-diseases-cird/
