Session Information
Date: Friday, November 6, 2020
Title: Patient Outcomes, Preferences, & Attitudes Poster I: RA, Spondyloarthritis, & OA
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Obesity is associated with higher disease activity in many rheumatologic diseases with evidence of improvement following bariatric surgery. Despite the impressive average weight loss values that occur after surgery, 10–30% of patients will have suboptimal weight loss or weight-regain. The RAPID3 on Multidimensional Health Assessment Questionnaire (MDHAQ), is a patient-reported, disease monitoring index with 3 components: Function (FN), Pain (PN), and Global Health (GL). This longitudinal study explored predictors of improvement in RAPID3 and weight loss in rheumatology patients before and after bariatric surgery.
Methods: Rheumatology patients evaluated between 2012-2019 with documented RAPID3 scores were enrolled. Variables collected included demographics, BMI, and MDHAQ components at baseline/pre-surgery (T1), 6 month post-surgery (T2) and 12 month post-surgery (T3). For Model 1, we conducted a univariate binary logistic regression analysis with clinically significant improvement in RAPID3 (defined as decline of ≥3.6) between T1 and T2 as the dependent variable (DV). Predictor variables (PV) tested include age, education, comorbidities, T1 BMI, and TI MDHAQ. For Model 2, we performed a linear regression analysis for % change in BMI between T2 and T3 as the DV, and clinically significant change in RAPID3 index as the PV. Change in BMI of 5% was considered clinically relevant. A P value of ≤0.05 was considered significant on two-tailed tests.
Results: 33 patients were enrolled (97% women). 30.3% were Caucasian, 48.5% African American, and 21.2% Hispanic (Table 1). Mean BMI and RAPID3 Index at T1 were 45.8 and 15.0, respectively. Changes in BMI and RAPID3 at T2 and T3 are shown in Table 2. There were no differences in BMI or RAPID3 by race. T1 RAPID3 GL predicted attainment of a clinically significant improvement in RAPID3 at T2 (OR 1.42, 95% CI 1.02-1.98, p=0.04). T1 BMI or % change in BMI were not predictive of a clinically significant change in RAPID3 at T2. Subjects with clinically significant decreases in RAPID3 scores at T2, saw a 7.5% greater decline in BMI from T2 to T3 compared to those without significant decrease (β 0.075, 95% CI 0.033-0.117, p=0.0015). Nearly 30% decline in % BMI change from T2 to T3 was explained by clinically significant decrease in RAPID3 index (R-Sq 0.29) at T2 (Figure 1).
Conclusion: Higher pre-surgical MDHAQ GL score predicted clinically relevant improvements in RAPID3 index at 6 months post-bariatric surgery. Attaining significant improvement in RAPID3 index at 6 months was further predictive of clinically relevant decline in BMI at 12 months. A plausible mechanism involves reinforcement in patients’ behavioral changes as a result of perceptible health improvements. Longitudinal studies with larger numbers of patients will be required to see if improvements in RAPID3 leads to sustained weight loss, and whether this leads to improvement in their underlying rheumatological condition.
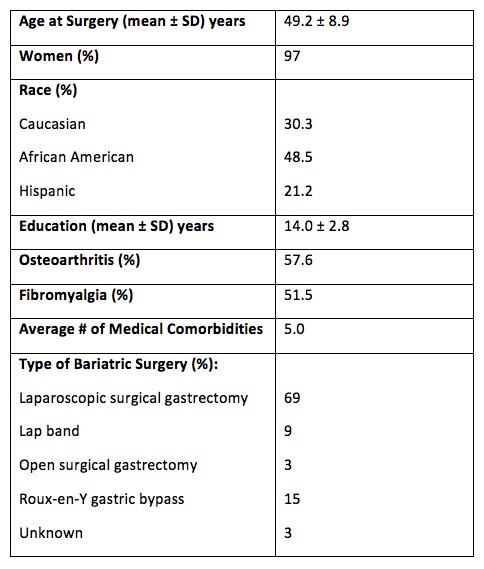 Patient Baseline Characteristics Prior to Bariatric Surgery
Patient Baseline Characteristics Prior to Bariatric Surgery
 Changes in BMI and RAPID3 Variables After Bariatric Surgery
Changes in BMI and RAPID3 Variables After Bariatric Surgery
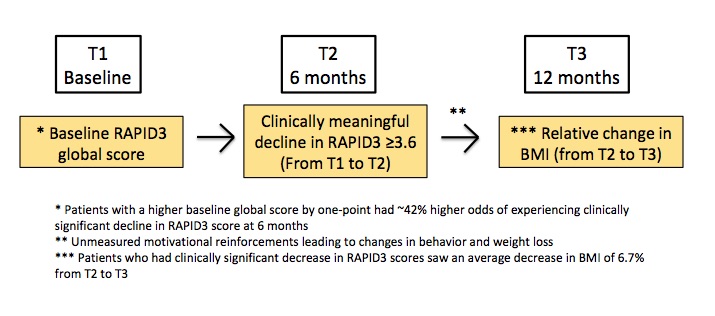 Two-Stage Model Showing Longitudinal Relationship Between T1 RAPID 3 Global Score, Clinically Significant Decline in RAPID3 at T2, and Subsequent BMI decline from T2 to T3
Two-Stage Model Showing Longitudinal Relationship Between T1 RAPID 3 Global Score, Clinically Significant Decline in RAPID3 at T2, and Subsequent BMI decline from T2 to T3
To cite this abstract in AMA style:
Byun J, Jolly M, Beck T, Hassan S. Routine Assessment of Patient Index Data (RAPID) 3 as a Predictor of Weight Reduction in Rheumatology Patients Undergoing Bariatric Surgery [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/routine-assessment-of-patient-index-data-rapid-3-as-a-predictor-of-weight-reduction-in-rheumatology-patients-undergoing-bariatric-surgery/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/routine-assessment-of-patient-index-data-rapid-3-as-a-predictor-of-weight-reduction-in-rheumatology-patients-undergoing-bariatric-surgery/
