Session Information
Date: Saturday, November 6, 2021
Title: Abstracts: Vasculitis – Non-ANCA-Associated & Related Disorders (0502–0507)
Session Type: Abstract Session
Session Time: 4:15PM-4:30PM
Background/Purpose: Giant cell arteritis (GCA) and polymyalgia rheumatica (PMR) are two chronic systemic inflammatory diseases that primarily affect elderly women. Both diseases can be complicated by inflammatory induced thrombosis, however the risk of thromboembolism among male patients with GCA and/or PMR is yet unknown. Due to the tight relationship between inflammation and thrombosis contributing to increased morbidity and mortality, we sought to determine the incidence rate of venous and arterial thrombotic events in patients with GCA and/or PMR among Veterans of the US. The objective of this study was to evaluate the risk of thromboembolism and retinal vascular events in GCA, PMR, and/or overlap of GCA with PMR compared to osteoarthritis (OA) in a Veteran’s based population.
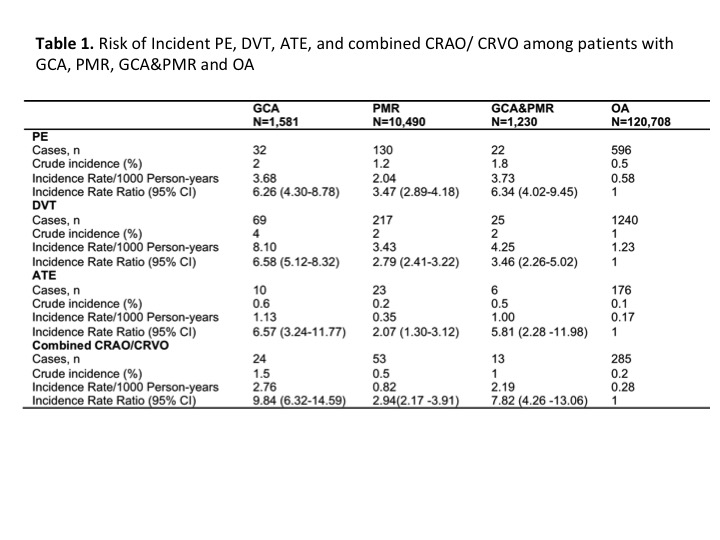
Methods: 1,581 patients with GCA, 10,940 with PMR, and 1,230 with GCA and PMR as well as 120,708 age- and sex-matched patients with OA, were identified in this retrospective study. Incidence rate ratios (IRR) of pulmonary embolism (PE), deep venous thrombosis (DVT), arterial thromboembolism of extremities (ATE), central retinal artery and vein occlusion (CRAO and CRVO) were calculated. We also calculated hazard ratios (HRs) of thromboembolic events in study groups, adjusting for independent risk factors of thromboembolism.
Results: Patients with GCA, PMR and GCA with PMR had higher IRs of all thromboembolic events as compared to patients with OA (Table 1). Patients with overlap of GCA and PMR had a lower risk of deep venous thrombosis (HR: 2.13, 95%CI:1.53-2.97, p< 0.001) and retinal vascular events (HR: 4.46, 95%CI:2.49-7.96, p< 0.001) as compared to patients with GCA (HR: 4.17, 95%CI:3.38-5.15, p< 0.001, and HR: 10.60, 95%CI: 7.56-14.86, p< 0.001, respectively), but a higher risk of retinal vascular events as compared to patients with PMR (HR: 2.33, 95%CI:1.75-3.11, p< 0.001) (Table 2).
Conclusion: The risk of thromboembolic events was higher in patients with GCA, PMR, and GCA with PMR compared to referenced population, and differed based on disease diagnosis. These findings may alert providers to be mindful of the importance for close monitoring of these patients for thromboembolic risk factors and may emphasize the need for a risk stratification strategy that would allow identification of high-risk patients.
To cite this abstract in AMA style:
Michailidou D, Zhang T, Stamatis P, Ng B. Risk of Venous and Arterial Thromboembolism in Patients with Giant Cell Arteritis And/or Polymyalgia Rheumatica: A Veterans Health Administration Population-Based Study in the United States [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/risk-of-venous-and-arterial-thromboembolism-in-patients-with-giant-cell-arteritis-and-or-polymyalgia-rheumatica-a-veterans-health-administration-population-based-study-in-the-united-states/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/risk-of-venous-and-arterial-thromboembolism-in-patients-with-giant-cell-arteritis-and-or-polymyalgia-rheumatica-a-veterans-health-administration-population-based-study-in-the-united-states/