Session Information
Date: Saturday, November 7, 2020
Title: Epidemiology & Public Health Poster II: OA, Osteoporosis, & Other Rheumatic Disease
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Hydroxychloroquine (HCQ) is used in the treatment of a wide variety of autoimmune diseases. HCQ retinopathy is a feared complication of long-term use. The reported prevalence of this complication increased with the advent of optical coherence tomography (OCT) or visual field assessment (VFA), and is estimated to be approximately 7.5% after five years of use. This led to guideline recommendation of using lower doses of HCQ. However, the reliance on prevalence rather than on incidence to predict the risk of developing a non-fatal and irreversible condition such as retinopathy leads to risk overestimation. To better estimate the risk of this complication, we estimated the incidence (risk) of retinopathy among new HCQ users.
Methods: A cohort of new HCQ users in a geographically defined 27-county region was identified using population-based research infrastructure. Prescription data was available starting in 2003 for one county and since 2010 for the rest of the counties. The patients were followed until HCQ toxicity incidence, migration out of the region, death or December 31, 2018. Medical records of these patients were reviewed for the development of HCQ retinopathy. HCQ retinopathy was defined based on characteristic paracentral visual field defects and parafoveal retinal photoreceptor layer changes on OCT. Indication for HCQ, demographics and risk factors for retinopathy were abstracted. Incidence rates were age‐ and/or sex‐adjusted to the estimated 2010 white population of the US. To compute 95% confidence intervals for incidence rates, it was assumed that the number of incident cases followed a Poisson distribution. The cumulative incidence rates after 4 years of HCQ use were estimated adjusting for the competing risk of death. Risk factors for HCQ retinopathy were estimated using Cox models.
Results: The study cohort identified 372 new HCQ users who had taken HCQ for four or more years. The average age was 54 years and 79% were female. The most common indications for HCQ were RA and SLE. The average follow up was 9.6 years after the first HCQ prescription (range 4.2 to 17.1). The mean dose in mg was 358.9, while the mean daily dose per weight was 4.6 mg/kg. Eight patients developed HCQ retinopathy, all were females and 88% were white. The majority used HCQ for RA treatment. The mean daily dose per weight was 5.9 mg/kg (Table 1). Table 2 references the risk of HCQ retinopathy. After five years of use, the risk was 0% and progressively increased up to 2.5% at ten years. Age at onset of therapy, daily dose per 100 mg, male sex, and presence of CKD did not increase the risk of retinopathy (Table 3). Those taking >5mg/kg of HCQ had a hazard ratio of 2.6 (0.64, 10.43) compared to those who took less than 5mg/kg, however this did not reach statistical significance.
Conclusion: The risk of HCQ retinopathy at ten years of use is lower compared to previous prevalence-based estimations. The number of cases was low for risk factor assessment; however, a dose higher than 5mg/kg may be associated with higher HCQ retinopathy risk.
 Table 1. Selected Study Population and Case Characteristics
Table 1. Selected Study Population and Case Characteristics
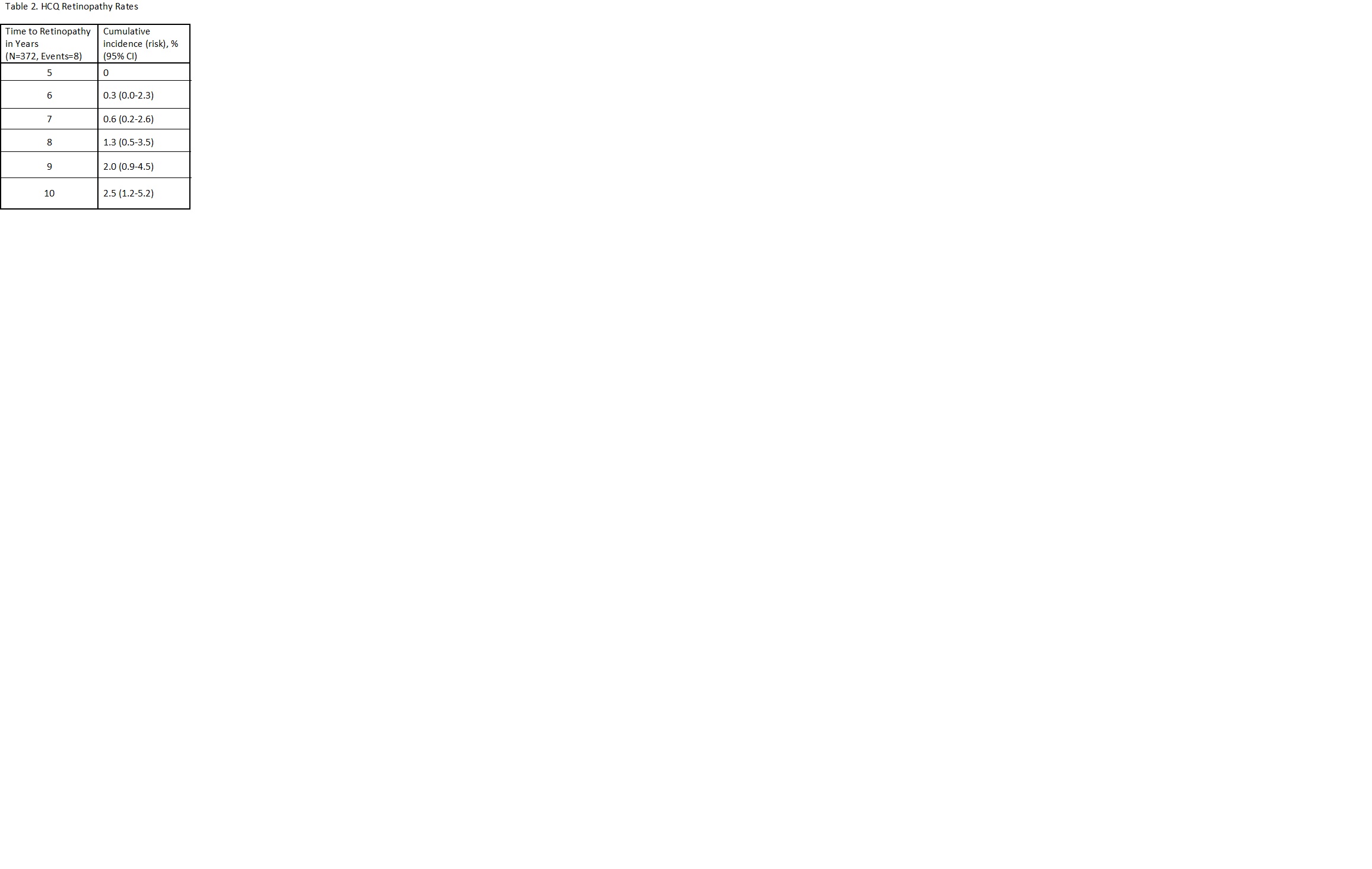 Table 2. HCQ Retinopathy Rates
Table 2. HCQ Retinopathy Rates
 Table 3. Risk factors for HCQ Retinopathy
Table 3. Risk factors for HCQ Retinopathy
To cite this abstract in AMA style:
Dabit J, Hocaoglu M, Moder K, Barkmeier A, Smith W, O'Byrne T, Crowson C, Duarte-Garcia A. Risk of Hydroxychloroquine Retinopathy in the Community [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/risk-of-hydroxychloroquine-retinopathy-in-the-community/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/risk-of-hydroxychloroquine-retinopathy-in-the-community/
