Session Information
Date: Tuesday, November 12, 2019
Title: 5T093: SLE – Clinical V: Emerging Knowledge of Current Treatments (2780–2785)
Session Type: ACR Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: Patients with systemic lupus erythematosus (SLE) have an increased risk for cardiovascular disease (CVD). SLE itself predisposes patients to accelerated atherosclerosis. In addition, the risk of CVD may be due to effects of drugs used to treat SLE, particularly glucocorticoid (GC). However, population-based studies assessing the risk of CVD associated with the use of GC with proper adjustment of time-varying confounders that might be also acting as intermediary variables in patients with newly diagnosed SLE are limited. We aim to address this question and the idea that recency of GC use may impact the effect.
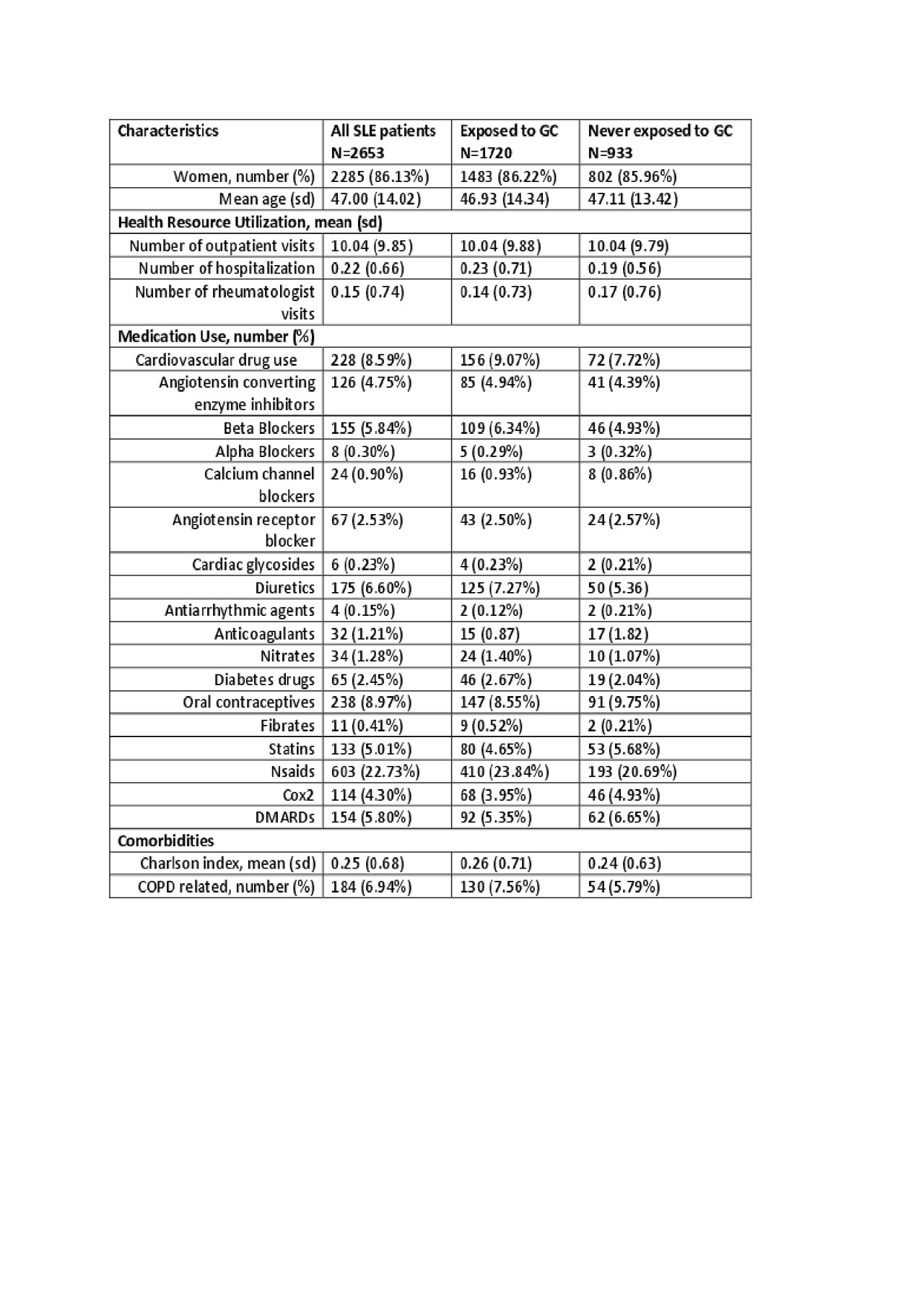
Methods: Our data included all outpatient and inpatient visits, demographic data, cancer registry and vital statistics from Jan 1990 to Mar 2015 and all dispensed medication from Sept 1995 to Mar 2015 in the province of British Columbia, Canada. Using a previously validated SLE case definition, we assembled an incident cohort of all SLE patients who received health care between January 01 1997 and March 31 2015 with no exposure to GC before SLE onset. CVD events (myocardial infarction (MI) or stroke) were identified using both hospitalization and vital statistics data. Individuals were followed until they experienced a CVD outcome, died, left BC, or follow-up ended, whichever occurred first. We used the marginal structure Cox model to estimate the impact of the GC initiation on the risk of CVD, adjusting for both baseline and time-dependent covariates (including health resource utilization and relevant medications (listed in table1)) that were updated every three months during follow-up. We defined GC exposure in four more ways: current use (yes/no), current dose (mg/day), cumulative dose (grams), cumulative duration (months). All were used as time-dependent variables. To permit the effect of a GC use in the past 180 days to vary by its recency, we created weighted versions of the cumulative dose and duration (i.e., straight-line, concave, convex, and half-normal weighting function). Cox proportional hazard models were used to estimate the risk of CVD of these GC exposure measures.
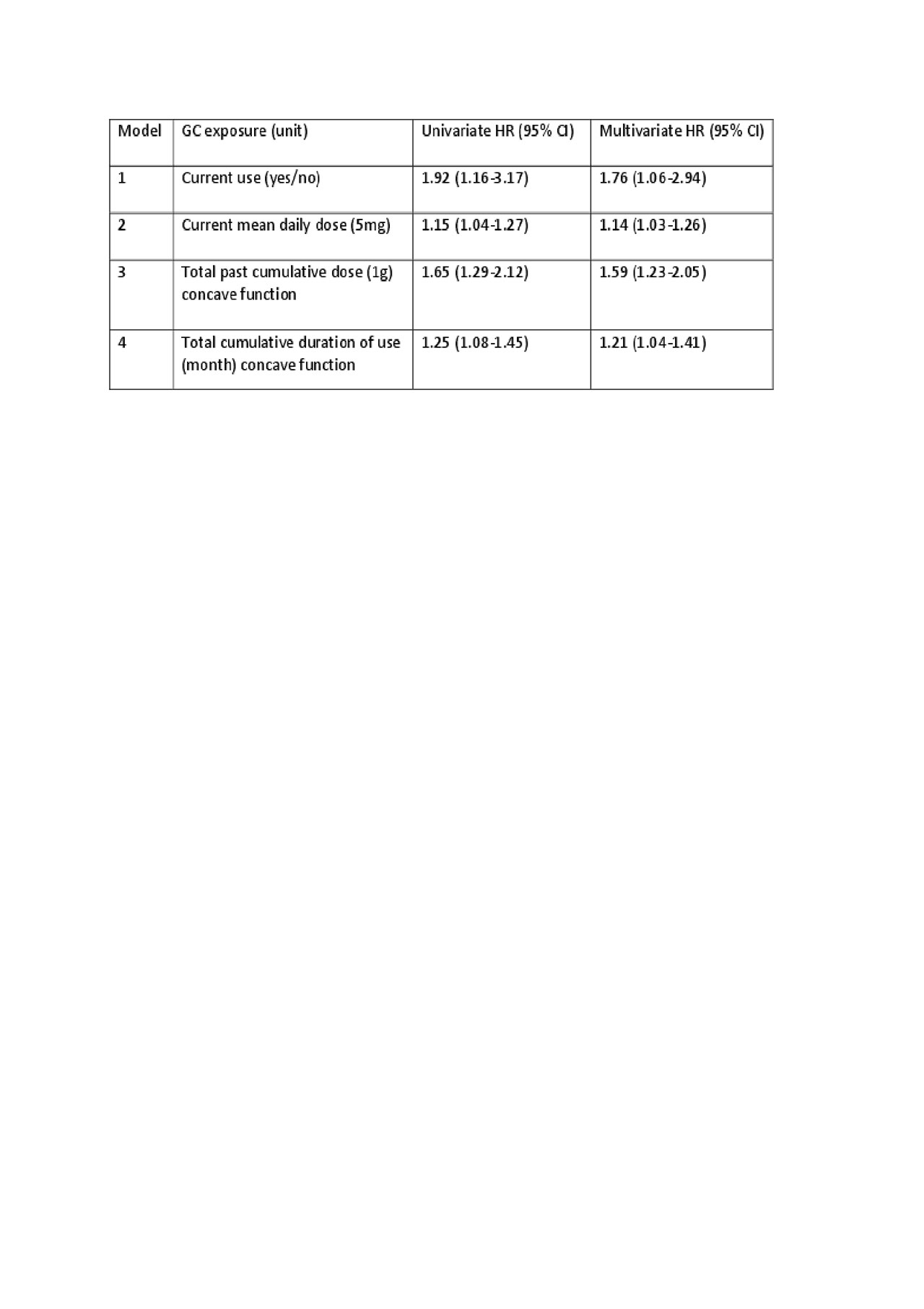
Results: We identified 2,653 incident SLE patients with no GC use history at baseline (mean age 47, 86% females). During follow-up, 1,720 (65%) received GC. GC users spend an average 15% of their follow-up time on GC with a median dose of 5 mg/day and a median duration per GC course of 29 days. During follow-up, we identified 108 CVD events (MI 69; stroke 45). Using marginal structure model, the hazard ratio (HR) after GC initiation was 1.82 (95%CI; 1.18-2.81) adjusted for baseline and time-dependent variables. Current GC use and current daily dose were associated with significantly increased risk of CVD (HR; 1.76 (95%CI; 1.06-2.94) and 1.14 (95%CI; 1.03-1.26)) (Table 2). Concave function for both cumulative dose and cumulative duration of use were selected as the best weighting function with the smallest AIC. Both of them were statistically significant (HR: 1.59 (95% CI; 1.23-2.05) and 1.21 (95% CI; 1.04-1.41)).
Conclusion: We found that the initiation of GC use is associated an 82% increased risk of CVD during follow-up. Higher risk of CVD is also associated with current GC use, higher current and cumulative GC dose and longer duration of GC use.
To cite this abstract in AMA style:
Li L, Xie H, Sayre E, Avina-Zubieta J. Risk of Cardiovascular Disease Associated with the Use of Glucocorticoids in Patients with Incident Systemic Lupus Erytematosus: A Population-based Study [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/risk-of-cardiovascular-disease-associated-with-the-use-of-glucocorticoids-in-patients-with-incident-systemic-lupus-erytematosus-a-population-based-study/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/risk-of-cardiovascular-disease-associated-with-the-use-of-glucocorticoids-in-patients-with-incident-systemic-lupus-erytematosus-a-population-based-study/