Session Information
Date: Monday, November 8, 2021
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster III: Outcomes (1257–1303)
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: Kidney biopsy is essential for the diagnosis and classification of lupus nephritis in patients with systemic lupus erythematosus (SLE). Even though the risk of bleeding-related complications is not low in such patients, data on the risk of percutaneous kidney biopsy in SLE patients are limited. Thus, we investigated the rate of bleeding-related complications and examined the risk factors for complications of kidney biopsy in patients with SLE.
Methods: We retrospectively reviewed the medical records of SLE patients who underwent ultrasound-guided percutaneous kidney biopsy between 2002 and 2020 at a tertiary referral center. Major complications included bleeding events that required interventions (e.g., blood transfusion, angiographic embolization, surgery) after biopsy. Minor complications included hematoma, oozing at the biopsy site, and passing hematuria without a need for intervention. Statistical analysis with a multivariate logistic regression model was performed to identify the risk factors associated with complications.
Results: In a total of 165 SLE patients, the rate of overall bleeding-related complication after kidney biopsy was 25% (major: 8%, minor: 17%). In terms of the details of major complications, 86% (12/14) of patients needed a blood transfusion alone without embolization or surgery, and the remaining two patients needed embolization for bleeding control. Patients with any kind of complication had a significantly lower platelet level than did those without complications (p< 0.001). Univariate analysis showed that the levels of hemoglobin (OR 0.81; 95% CI, 0.66–0.99), platelet (OR 0.99; 95% CI, 0.99–1.00), aPTT (OR 1.05; 95% CI, 1.00–1.11), and proteinuria (OR 1.00; 95% CI, 1.00–1.00) were significantly associated with the risk of complications. Multivariate analysis revealed that low platelet count (OR 0.99; 95% CI, 0.98–0.99) was significantly associated with the risk of bleeding-related complications after kidney biopsy.
Conclusion: Percutaneous kidney biopsy was accompanied by the risk of bleeding-related complications, although the majority of events did not require vascular intervention for bleeding control. Low levels of platelet counts had a significantly increased risk of complications after kidney biopsy in patients with SLE.
 BMI: body mass index; sBP: systolic blood pressure; PT INR : prothrombin time international normalized ratio; aPTT: activated partial thromboplastin time; eGFR: estimated glomerular filtration rate; C3/C4: complement 3/4ESR: erythrocyte sedimentation rate; ACA: anticentromere antibody; B2-GPI: Beta_2-glycoprotein I antibody ACEi/ARB: angiotensin converting enzyme inhibitor/angiotensin receptor blocker ISN/RPS: International Society of Nephrology and Renal Pathology Society
BMI: body mass index; sBP: systolic blood pressure; PT INR : prothrombin time international normalized ratio; aPTT: activated partial thromboplastin time; eGFR: estimated glomerular filtration rate; C3/C4: complement 3/4ESR: erythrocyte sedimentation rate; ACA: anticentromere antibody; B2-GPI: Beta_2-glycoprotein I antibody ACEi/ARB: angiotensin converting enzyme inhibitor/angiotensin receptor blocker ISN/RPS: International Society of Nephrology and Renal Pathology Society
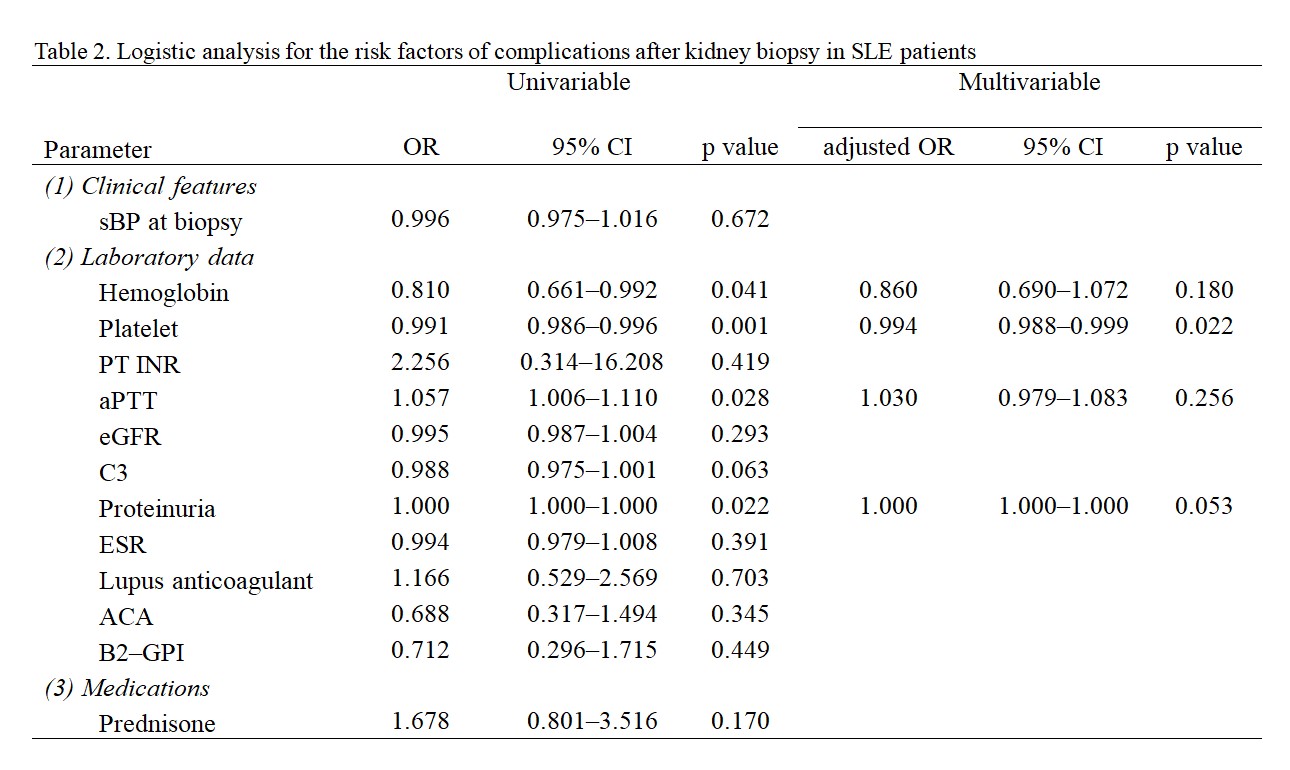 sBP: systolic blood pressure; PT INR : prothrombin time international normalized ratio; aPTT: activated partial thromboplastin time; eGFR: estimated glomerular filtration rate; C3: complement 3 ESR: erythrocyte sedimentation rate; ACA: anticentromere antibody; B2-GPI: Beta_2-glycoprotein I antibody
sBP: systolic blood pressure; PT INR : prothrombin time international normalized ratio; aPTT: activated partial thromboplastin time; eGFR: estimated glomerular filtration rate; C3: complement 3 ESR: erythrocyte sedimentation rate; ACA: anticentromere antibody; B2-GPI: Beta_2-glycoprotein I antibody
To cite this abstract in AMA style:
Kang E, Oh J, Ahn S, Kim Y, Lee C, Yoo B, Hong S. Risk of Bleeding-related Complications After Kidney Biopsy in Patients with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/risk-of-bleeding-related-complications-after-kidney-biopsy-in-patients-with-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/risk-of-bleeding-related-complications-after-kidney-biopsy-in-patients-with-systemic-lupus-erythematosus/
