Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Prognostic factors for pain persistence after total joint replacement (TJR) in osteoarthritis (OA) have been repeatedly proposed. These factors are commonly considered to act independently, unrelated to each other, even with regard to the various pain intensity measures used. Here, we purpose that pain outcomes post-TJR relate to different aspects of the pain experience and explore how predictive modeling may lead to different results regarding pain persistence risk factors.
Methods: We conducted a prospective longitudinal study of knee and hip OA patients, assessing multiple measures by questionnaires of quality, mood, affect, health and quality of life, together with radiographic evaluation and performance-based tasks before and 6 months after TJR. These factors were firstly used in a principal component analysis (PCA), thus applying a data reduction technique, and then used to build multivariate regression models (stepwise hierarchical regression: α-to-enter 0.05 and α-to-remove 0.10) for four distinct pain intensity outcomes (NRS, BPI Pain, KOOS pain and SF-36 pain). All pain outcomes were modeled at baseline and post-surgery, both as absolute value and also as score change (% residual pain) for the latest.
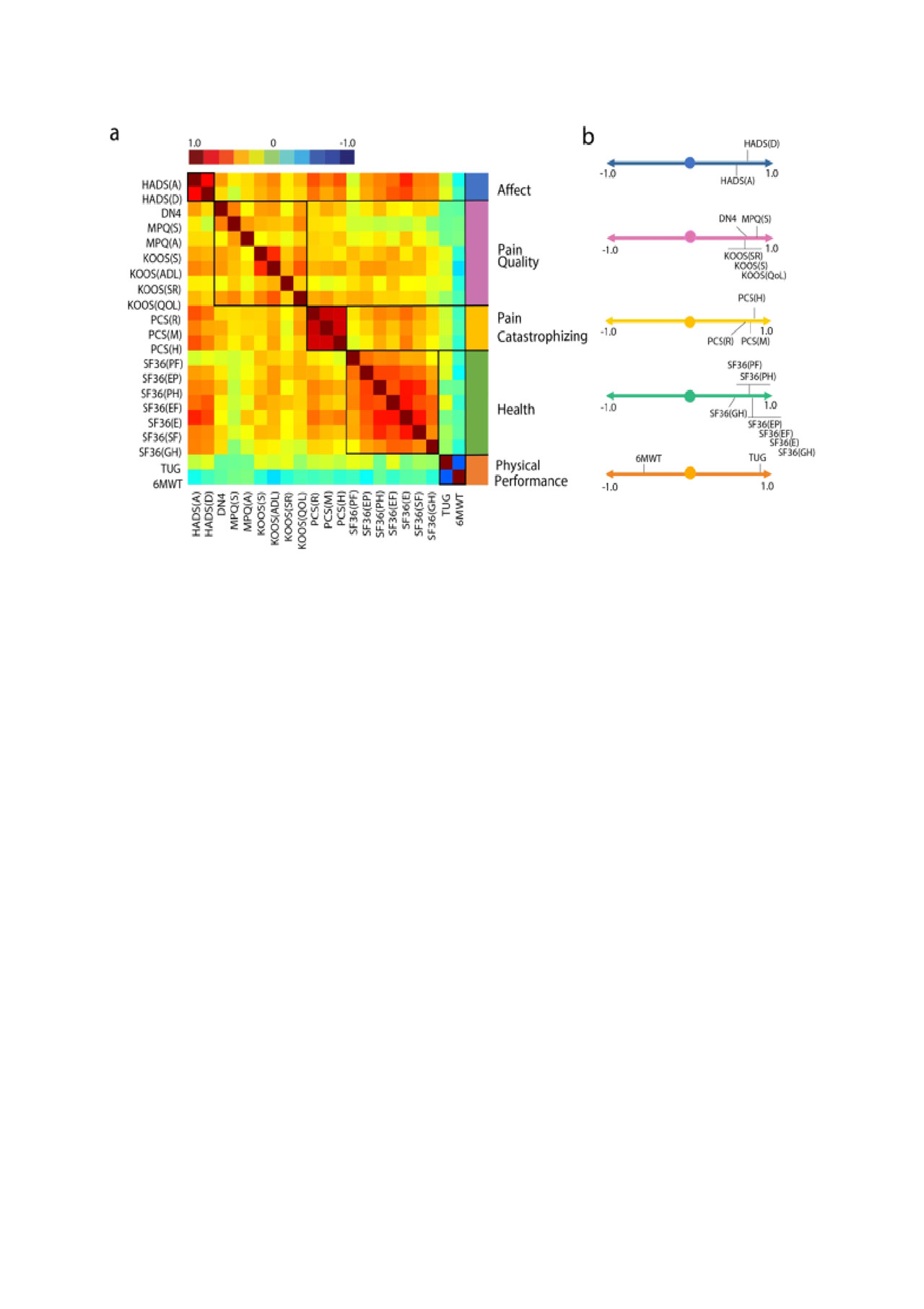
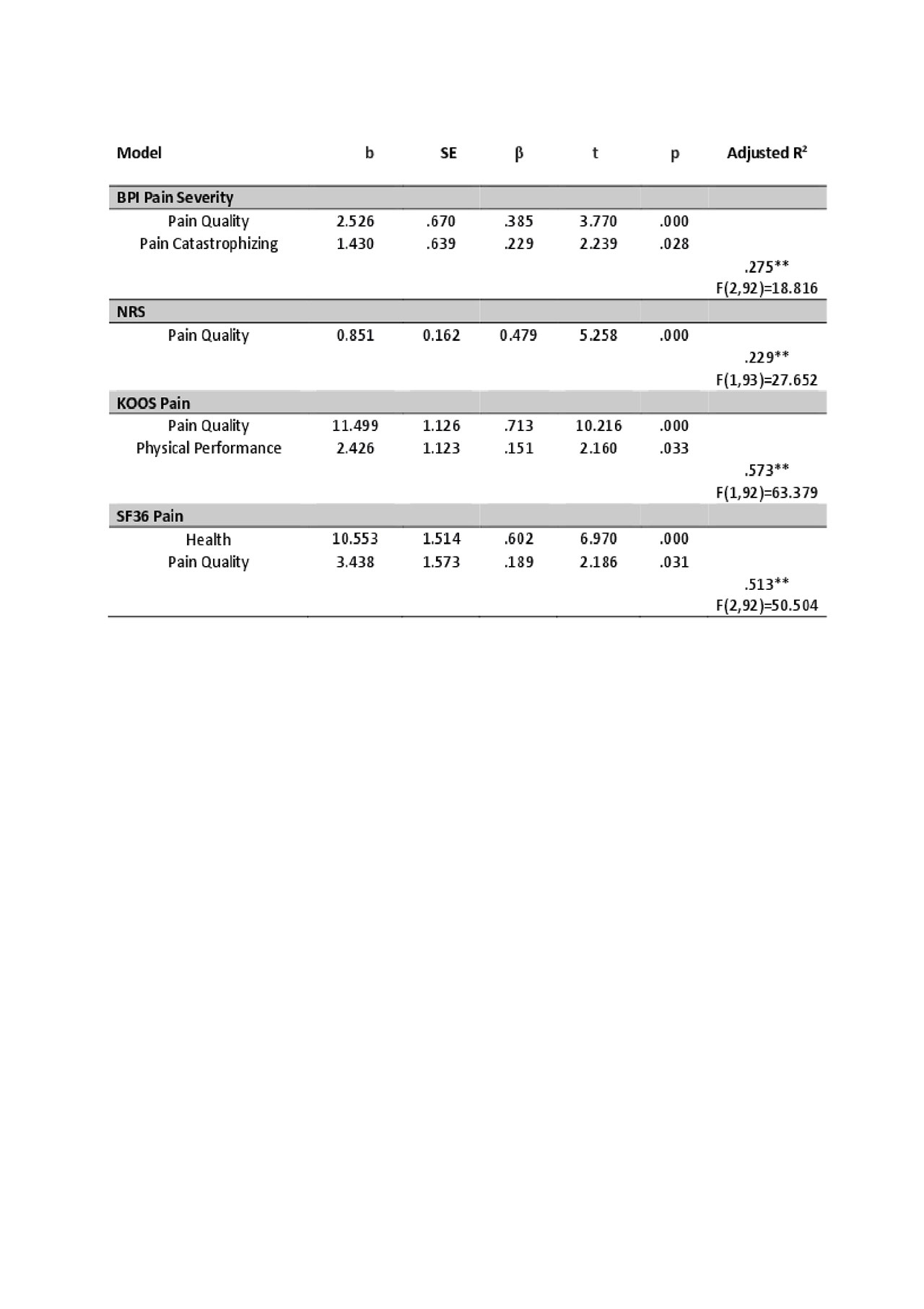
Results: A total of 84 knee OA and 24 hip OA patients completed the study. For the four pain scales, pairwise comparisons revealed that pain intensity estimates were significantly lower only for BPI pain severity at baseline (mean differences [SD]: NRS: -1.72 [-2.44, -0.99], KOOS/HOOS: -1.436 [-2.158, -0.71], SF36: -2.06 [-2.78, -1.4], p< 0.001) and higher 6 months post-surgery with SF-36 pain (NRS: 1.038 [0.23,1,81], BPI: 1.354 [0.57,2.14], p< 0.003). The PCA for questionnaire variables identified 5 distinct components, accounting for 70% of the variability of the data. These were labeled accordingly to its factor loadings as pain quality, affect, catastrophizing, health and physical performance (Figure 1). Hierarchical models showed pain quality as the common dominant factor accounting for higher pain intensity throughout all scales pre-surgery, with additional influences for each outcome (Table 1). Different models were elicited for absolute versus relative pain intensity (change in pain vs pre-TJR) after surgery, with the variance explained by each model being overall lower for change in pain. Again, explanatory variables were also distinct considering the four different pain outcome measures (Table 2).
Conclusion: These results demonstrate that different pain scales relate to distinct facts of the pain experience, resulting in defining distinct prognostic factors for persistence of pain post-TJR. These models allow for distinction between post-TJR absolute pain levels vs degree of improvement from the pre-op state. Structured and comprehensive methodological approaches regarding pain metrics are necessary in order to better understand and derive clinical prognostic factors in post-TJR pain.
a. Correlation matrix ordered based on principal component analysis results -Pearson’s r represented by color bar-. The five identified components were labeled according to membership properties. b. Factor loadings are shown for the five components. 6MWT, six minute walking test; DN4, The Neuropathic Pain 4 questions; HADS-A-, The Hospital Anxiety and Depression Scale, Anxiety; HADS-D-, The Hospital Anxiety and Depression Scale, Depression; KOOS, Knee Injury and Osteoarthritis Outcome Score, -ADL – Function in daily living-, -S -Knee Symptoms-, -SR – Function in sport and recreation-, -QOL – knee related quality of life-; MPQ, McGill Pain Questionnaire, -A – Affective score- -S – Sensory score-; PCS, Pain Catastrophizing Scale, -R – Rumination subscale-, -M – Magnification subscale-, -H – Helplessness subscale-; SF36, Short-form -36- Health Survey, -PF – Physical Functioning-, -PH – physical role functioning-, -EP – emotional role functioning-, -EF – energy/fatigue-, -E – emotional well-being-, -SF – social functioning-, -GH – general health-; TUG, Timed -up and go test.
Displayed statistics are from the final step of each model. b, unstandardized regression coefficient; SE, standard error; β, standardized regression coefficient; F, obtained F-value; t, obtained t-value; R2, proportion of variance explained. * p ≤ 0.05, **p ≤ 0.01. Displayed statistics are from the final step for each dependent variable. BPI Severity, Brief Pain Inventory Pain: severity subscale; HOOS Pain, Hip Injury and Osteoarthritis Outcome Score: pain subscale; NRS, Numeric Rating Scale; SF36 Pain, Short-form -36- Health Survey: pain subscale.
b, unstandardized regression coefficient; SE, standard error; β, standardized regression coefficient; F, obtain F-value; t, obtained t-value; R2, proportion variance explained. Gender: male coded as 0, female coded as 1. * p ≤ 0.05, **p ≤ 0.01. Displayed statistics are from the final step for each dependent variable.
BPI Severity, Brief Pain Inventory Pain: severity subscale; HOOS Pain, Hip Injury and Osteoarthritis Outcome Score: pain subscale; NRS, Numeric Rating Scale; SF36 Pain, Short-form -36- Health Survey: pain subscale.
To cite this abstract in AMA style:
Barroso J, Wakaizumi K, Schnitzer T, Galhardo V, Apkarian A. Risk Factors for Pain After Total Joint Replacement in Osteoarthritis: Different Pain Measures, Distinct Predictors? [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/risk-factors-for-pain-after-total-joint-replacement-in-osteoarthritis-different-pain-measures-distinct-predictors/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/risk-factors-for-pain-after-total-joint-replacement-in-osteoarthritis-different-pain-measures-distinct-predictors/