Session Information
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose:
Non-traumatic osteonecrosis (ON) is a well-recognized complication in systemic lupus erythematosus (SLE). The reported symptomatic ON prevalence is 10-15% and as high as 44% when including asymptomatic lesions. ON causes disability and affects quality of life (QoL). Bones collapse from ON has serious clinical implications and may lead to severe joint damage requiring total joint arthroplasty (TJA). The aim of this study was to identify specific risk factors for ON in SLE patients, in order to better guide monitoring of this debilitating complication.
Methods:
A systematic review was conducted using MEDLINE, PUBMED and EMBASE, searching to February 2015 using the MeSH terms “Osteonecrosis”, “Systemic lupus erythematosus” and synonymous text words. Randomized controlled trials (RCT), case control, cohort and cross sectional studies reporting at least one risk factor for ON were included. Risk factors for ON in SLE patients were compiled. The quality of evidence of each risk factor was assessed using the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) method. The quality of each study was assessed using the Newcastle-Ottawa scale (NOS).
Results:
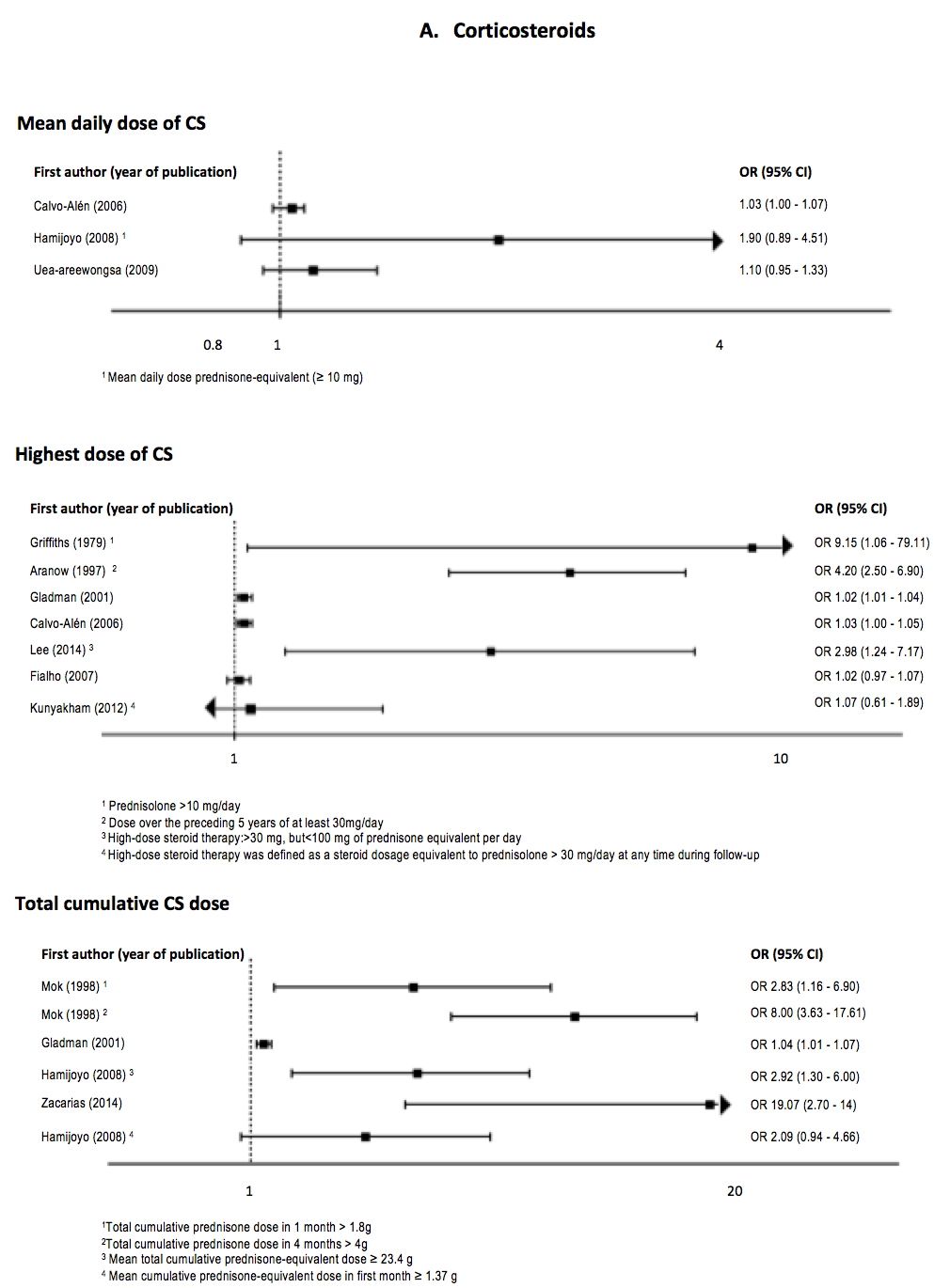
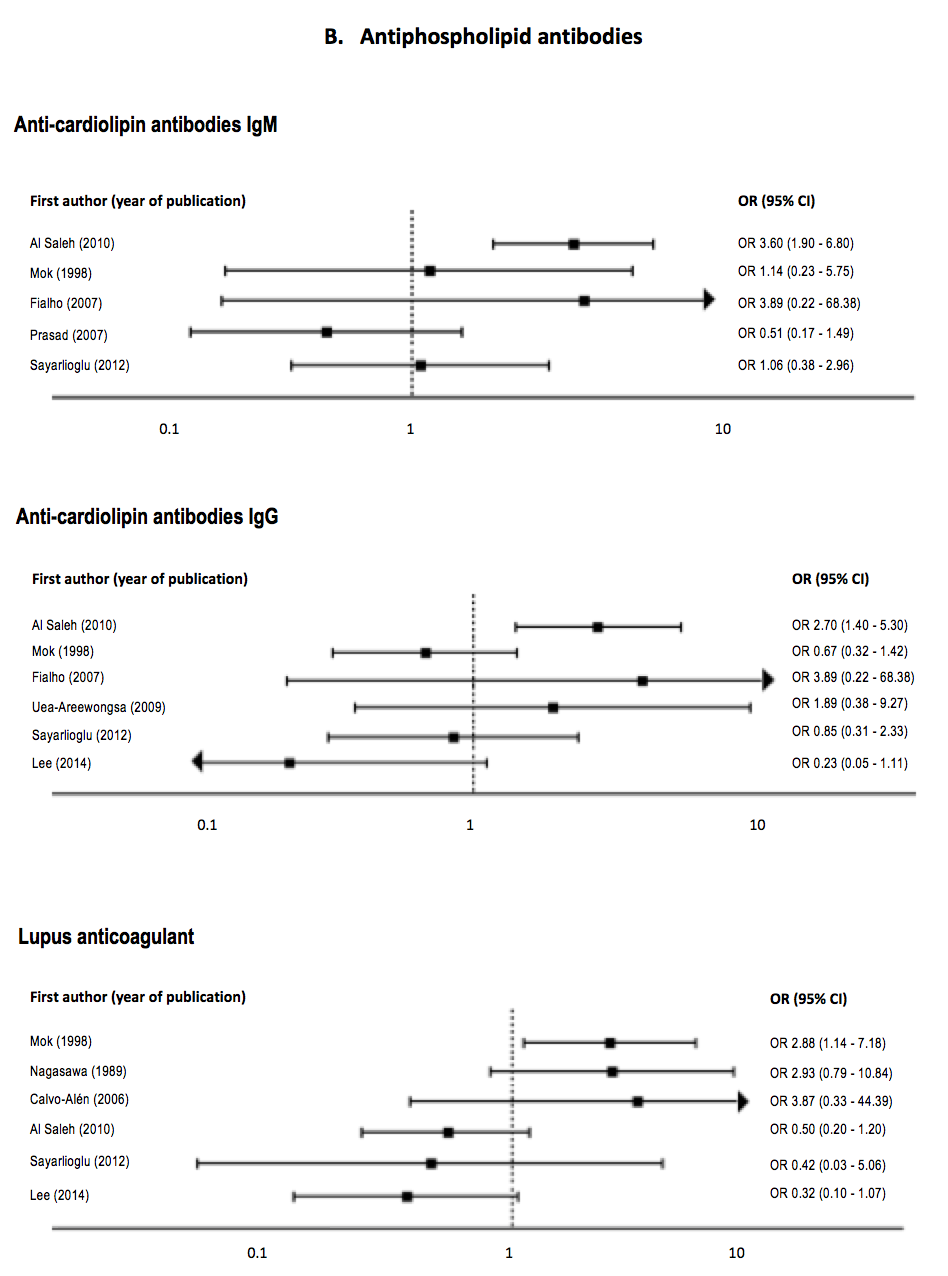
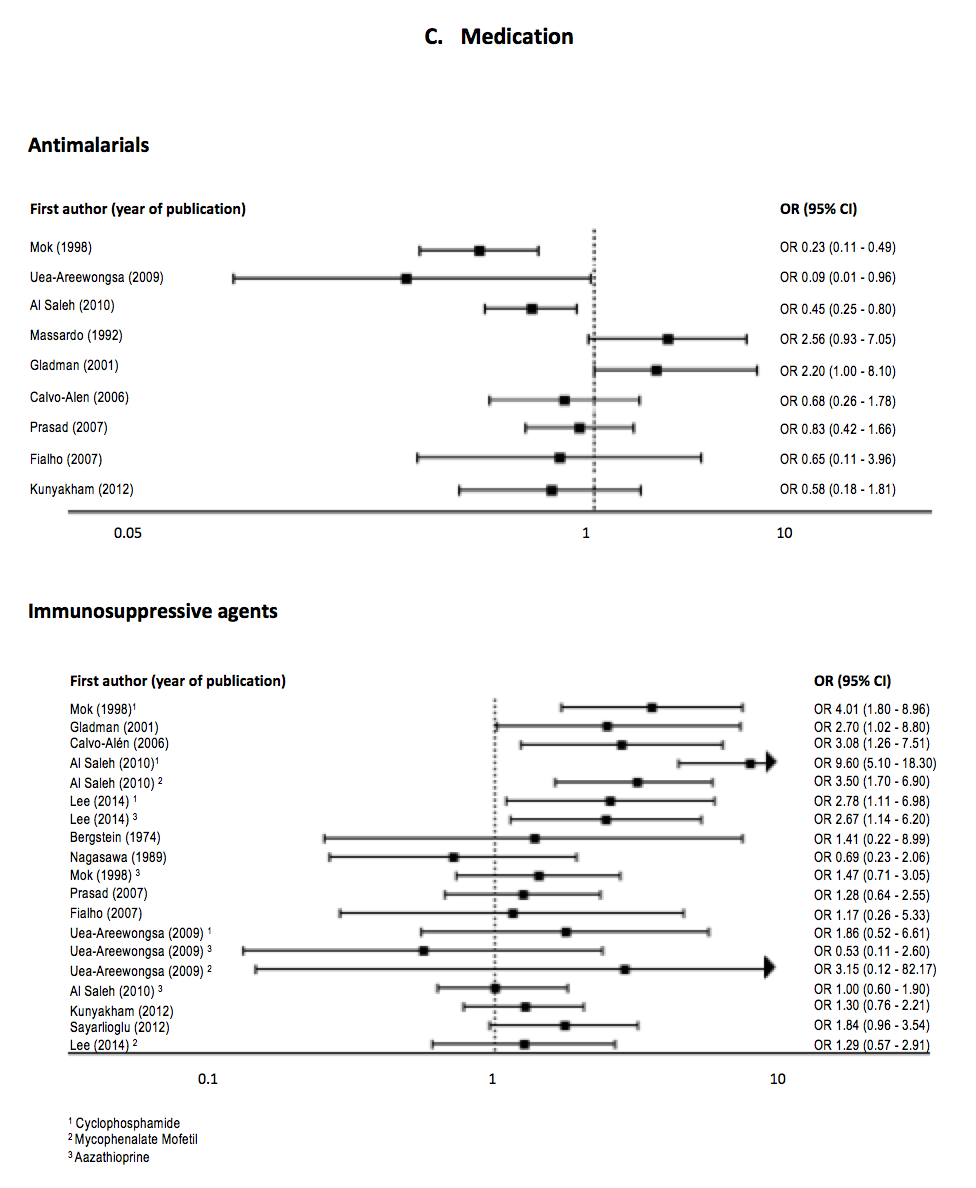
Of the 536 references yielded, 28 met inclusion criteria. In the literature, the major risk factor associated with ON remains the use of corticosteroids (CS). ON is much more prevalent in SLE than in other systemic conditions requiring the use of CS, suggesting that the use of CS is not the only factor. Multiple other clinical variables were evaluated in studies, including disease activity, arthritis, neuropsychiatric SLE, Raynaud’s phenomenon, vasculitis, serositis, gastrointestinal involvement, hypertension, oral ulcers, renal disease, alopecia, antiphospholipid antibodies, antimalarials and immunosuppressive agents. However, for those other risk factors, the research evidence was weak and the association between these variables and the development of ON was controversial (see forest plots).
Conclusion:
Based on the best evidence available, CS use is the only modifiable risk factor clearly associated with ON in SLE patients. Physicians should maintain a high index of suspicion for ON in SLE patients, especially with any history of CS exposure. We suggest adopting a preventive strategy with a judicious use of CS.
To cite this abstract in AMA style:
Hussein S, Suitner M, Baril-Dionne A, Popescu ML, Santesso N, Keeling SO, Pope JE, Fifi-Mah A, Bourré-Tessier J. Risk Factors for Osteonecrosis in Systemic Lupus Erythematosus: A Systematic Review [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/risk-factors-for-osteonecrosis-in-systemic-lupus-erythematosus-a-systematic-review/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/risk-factors-for-osteonecrosis-in-systemic-lupus-erythematosus-a-systematic-review/