Session Information
Date: Sunday, November 12, 2023
Title: (0673–0690) Vasculitis – ANCA-Associated Poster I: Treatment Outcomes
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: B-cell depletion induced by rituximab (RTX) in ANCA-associated vasculitis (AAV) is a risk factor for hypogammaglobulinemia. Aggregating data on the kinetics of gammaglobulin levels during RTX and its association with the risk of relapse and serious infection is of interest.
Methods: We conducted a retrospective single-centre cohort study including patients with granulomatosis with polyangiitis and microscopic polyangiitis who received RTX maintenance therapy between January 2010 and November 2022. Gammaglobulin levels were measured before induction therapy (month -6), at initiation of RTX maintenance therapy (month 0) and every 6 months during maintenance therapy. Patients were categorized into several groups: (1) patients with gammaglobulin levels < 6 g/L at initiation month 0; (2) patients with gammaglobulin decline between induction and initiation of maintenance therapy >25%; and finally (3) patients responding to both criteria simultaneously. Our primary objective was to assess the impact of gammaglobulin decline on the risk of vasculitis relapse and serious infections.
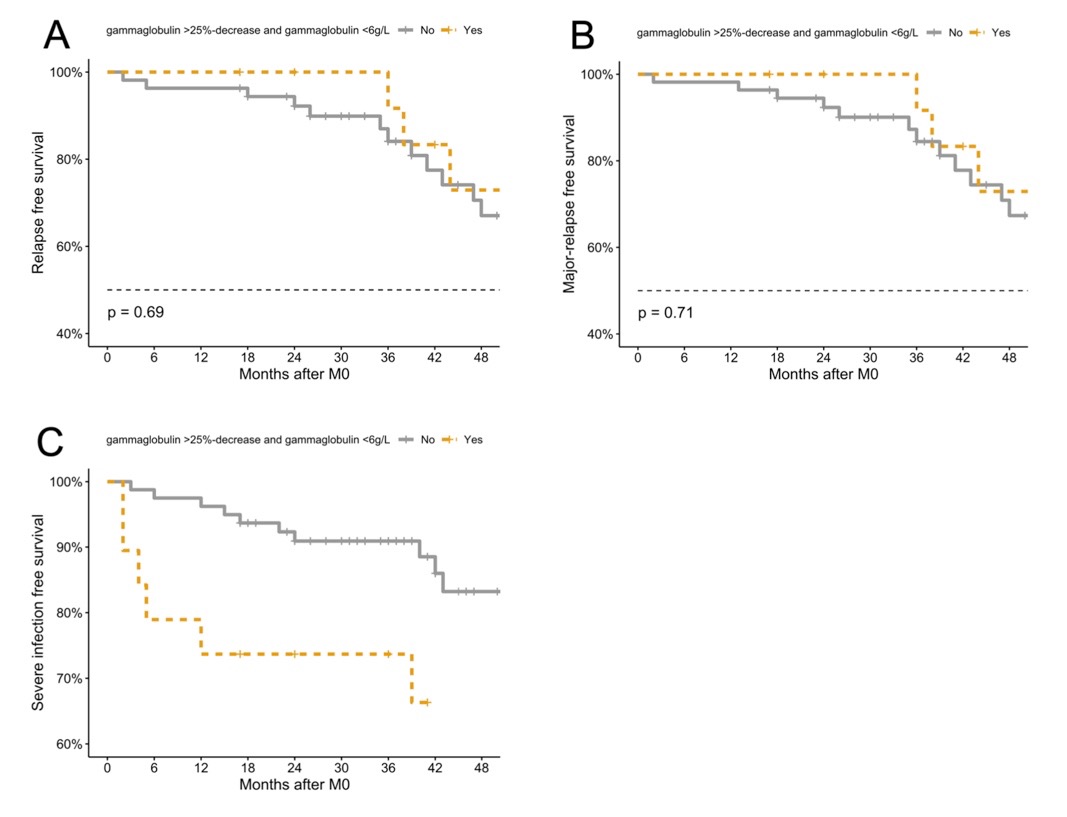
Results: We included 98 patients, all of whom fulfilled the ACR/EULAR classification criteria of AAV. The median gammaglobulin level at initiation of induction therapy was 10.4 g/L (IQR 8.4–12.9) and it significantly decreased to 7.5 g/L (5.9-8.8) at initiation of maintenance therapy with a median decrease of -25% (IQR -13.8 – -42.4). Gammaglobulin levels remained stable throughout follow-up (Figure 1). Factors associated with gammaglobulin level decline >25% and gammaglobulin level < 6 g/L after induction were age > 60 years (OR 4.1; 95%CI 1.2–14.7), baseline gammaglobulin levels < 10 g/L (OR 5.9; 95%CI 1.7–25.4) and use of pulses of methylprednisolone at induction (OR 4.7; 95%CI 1.4–2). Gammaglobulin decline was not associated with the risk of relapse. In contrast, serious infection-free survival was significantly poorer in patients with both gammaglobulin < 6 g/L and gammaglobulin decline >25% (adjusted HR 2.3; 95%CI 1.0–5.1) (Figure 2) and in those who received pulses of methylprednisolone (HR 5.6; 95%CI 2.3–13.4) (Table 1).
Conclusion: Older age, low gammaglobulin levels and pulses of methylprednisolone at induction are associated with greater gammaglobulin decline after induction. Although it is not associated with a lower risk of vasculitis relapse, gammaglobulin decline is associated with an increased risk of serious infections.
To cite this abstract in AMA style:
LIBERATORE J, Nguyen Y, HADJADJ J, Cohen P, Mouthon L, Puéchal X, Guillevin L, Terrier B. Risk Factors for Hypogammaglobulinemia and Association with Relapse and Severe Infections in ANCA-Associated Vasculitis: A Retrospective Single-Centre Cohort Study [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/risk-factors-for-hypogammaglobulinemia-and-association-with-relapse-and-severe-infections-in-anca-associated-vasculitis-a-retrospective-single-centre-cohort-study/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/risk-factors-for-hypogammaglobulinemia-and-association-with-relapse-and-severe-infections-in-anca-associated-vasculitis-a-retrospective-single-centre-cohort-study/