Session Information
Date: Sunday, November 8, 2020
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Interstitial lung disease (ILD) is a frequent complication of RA and is associated with increased morbidity and mortality.1 Previous studies have shown variability in risk factors for RA-associated ILD (RA-ILD).1,2 The objective of this analysis was to systematically evaluate the risk factors of RA-ILD in a real-world population of patients with RA.
Methods: Patient demographic and disease characteristics were retrospectively analyzed following data extraction from the Discus Analytics JointMan database, a large US electronic medical records-based dataset. Adults with an RA diagnosis (International Classification of Disease, Ninth Revision, Clinical Modification [ICD-9-CM] code: 714.0; ICD, Tenth Revision, CM [ICD-10-CM] codes: M05, M06) between January 1, 2009 and September 20, 2019, ≥1 visit after the initial visit date, no diagnosis code for ILD prior to RA diagnosis and no diagnosis code for drug-induced ILD at any time during the study period were included in the analysis. Patients with ILD were identified by ICD diagnosis codes (ICD-9-CM codes: 516.0, 516.2, 516.3, 516.4, 516.5, 516.8, 516.9; ICD-10-CM codes: J84.0, J84.1, J84.2, J84.81, J84.82, J84.83, J84.89, J84.9) or by provider indication. Potential predictors of RA-ILD were analyzed by Cox regression model. Patient demographic and co-morbid conditions were collected at baseline (defined as 6 months prior to or on date of initial RA diagnosis). RA characteristics were identified during and after the initial RA diagnosis and were controlled as time-varying covariates in the Cox model. Significance was set at p< 0.05.
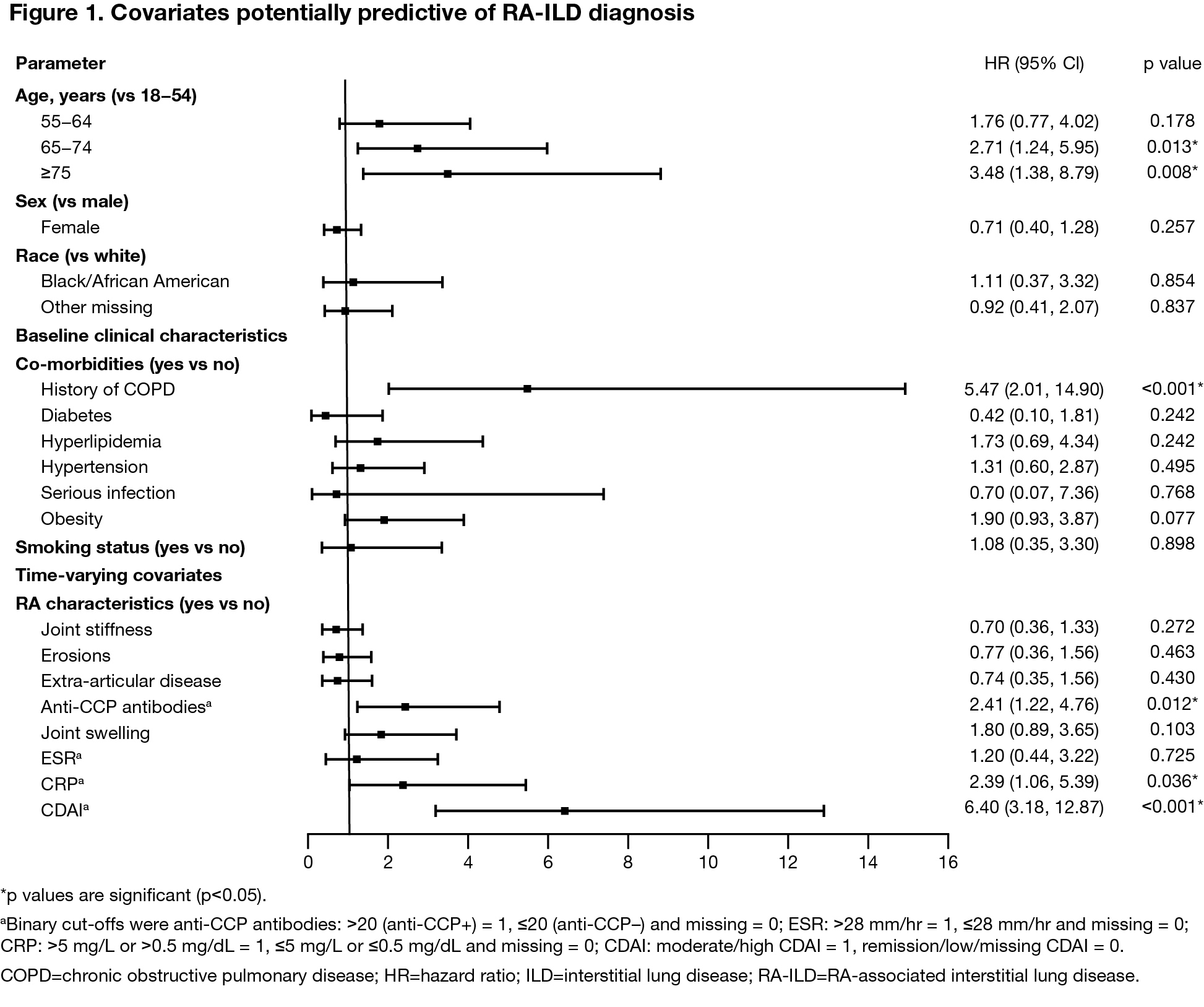
Results: Of the 5817 patients included, 5612 had RA only and 205 had RA-ILD. Several baseline differences between patients with and without ILD were identified: a greater proportion of patients with RA-ILD vs RA only were older, male, of white race, had a history of chronic obstructive pulmonary disease (COPD) and had more severe and more active RA than did patients with RA only (Table 1).3 Cox multivariate regression analysis showed older age ( >65 years old) and a history of COPD at baseline to be risk factors for developing ILD (Figure 1). Additionally, several time-varying covariates (anti-CCP positivity, CRP >5 mg/L and a moderate-to-high CDAI score) were also shown to be predictive of developing ILD.
Conclusion: In this large, real-world analysis of patients with RA, several risk factors for RA-ILD were identified: age, COPD, anti-CCP+, CRP and CDAI score. Recognition of these risk factors may lead to improved identification and a tailored approach to treatment of RA-ILD.
References:
- Spagnolo P, et al. Arthritis Rheumatol 2018;70:1544–1554.
- Kiely P, et al. BMJ Open 2019:9:e028466.
- Zhuo J, et al. Ann Rheum Dis 2020;79:24-25 (abstract OP0035).
Medical writing: Rachel Rankin (Caudex).
To cite this abstract in AMA style:
Zhuo J, Zhang Q, Knapp K, Wang Y, Gutierrez C, He D, Xie L, Lama S, Craig G. Risk Factors Associated with Interstitial Lung Disease in Patients with RA: Findings from a Retrospective Healthcare Database Analysis [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/risk-factors-associated-with-interstitial-lung-disease-in-patients-with-ra-findings-from-a-retrospective-healthcare-database-analysis/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/risk-factors-associated-with-interstitial-lung-disease-in-patients-with-ra-findings-from-a-retrospective-healthcare-database-analysis/