Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: As initial COVID-19 infections become nearly ubiquitous and the available prevention and treatment strategies evolve, patients with systemic autoimmune rheumatic diseases (SARDs) may be particularly vulnerable to repeat infections due to immunosuppression. However, no studies have investigated the risk factors and outcomes of repeat COVID-19 infections among patients with SARDs.
Methods: We performed a case-control study investigating risk factors and outcomes of repeat COVID-19 infections among SARD patients at a large healthcare system. All COVID-19 infections were systematically identified from positive PCR tests, patient-reported rapid antigen tests, or physician referral (3/15/2020 through 10/17/2022). SARD diagnosis was confirmed by a medical record review. The index date was the date of repeat COVID-19 infection, defined as a second infection >60 days after the initial infection. Controls had one COVID-19 infection as of their assigned index date (verified by medical record review and survey) and were matched to cases (up to 3:1) by date of first infection and duration between first infection and index date. We collected demographics, lifestyle, comorbidities, SARD features, and COVID-19 characteristics at initial infection and index date by medical record review. We used conditional logistic regression to identify associations with repeat COVID-19 infection, adjusting for potential confounders. We described the severity of repeat COVID-19 infection among cases.
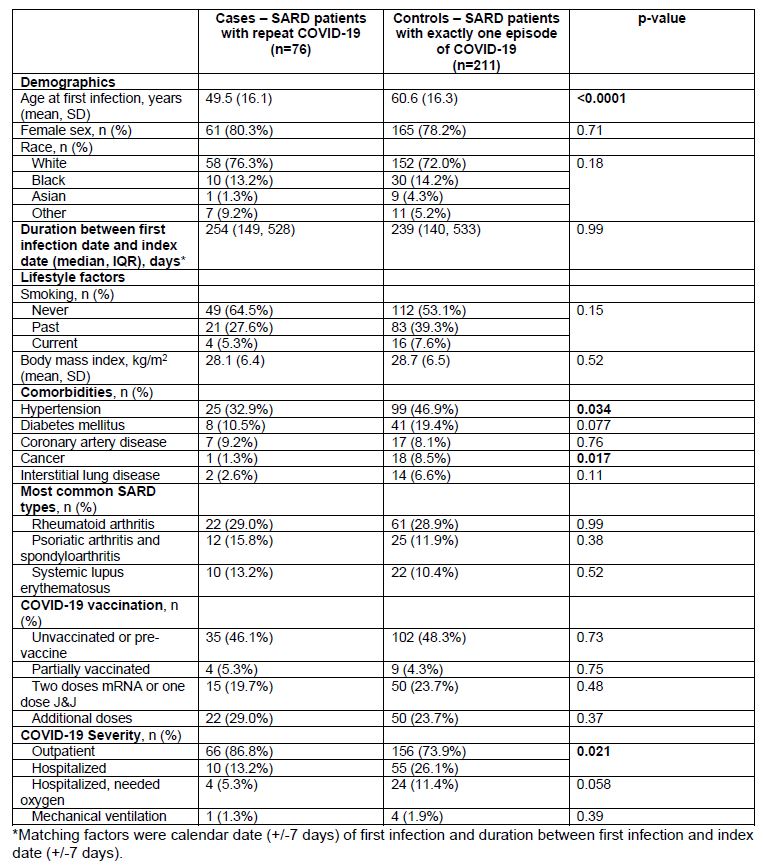
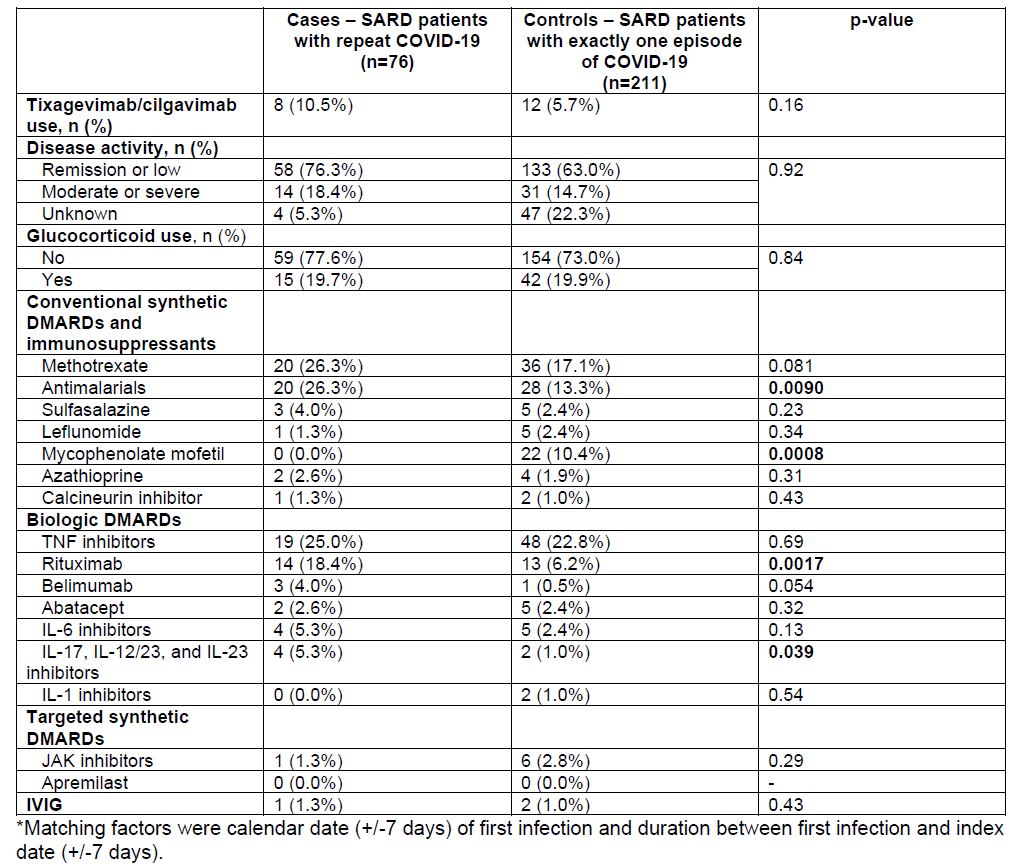
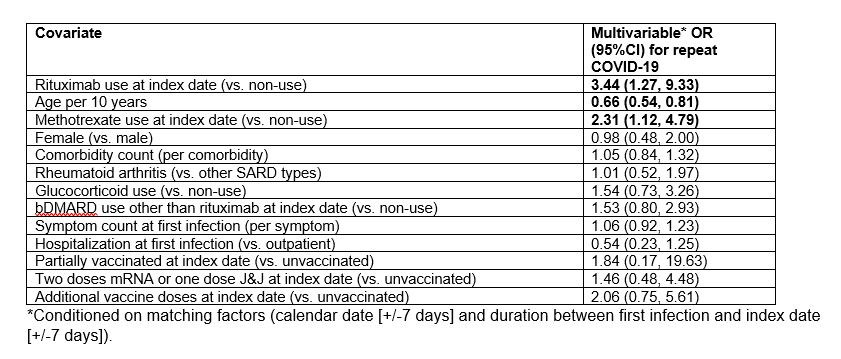
Results: Among 2,203 SARD patients with COVID-19, we identified 76 cases with repeat COVID-19 infection (80.3% female), matched to 211 matched controls (78.2% female) with no repeat infection. The most common SARD was RA, followed by psoriatic arthritis/spondyloarthritis and SLE (Table 1). At first infection, cases were younger (mean 49.5 vs. 60.6 years, p< 0.0001), less likely to have hypertension (32.9% vs. 46.9%, p=0.034), and less likely to have been hospitalized for COVID-19 (13.2% vs. 26.1%, p=0.021) than controls. At index date, cases were more likely than controls to be on antimalarials (26.3% vs. 13.3%, p=0.0090) or rituximab (18.4% vs. 6.2%, p=0.0017), but less likely to be on mycophenolate mofetil (0% vs. 10.4%, p=0.0008; Table 2). In the multivariable model, rituximab use vs. non-use (OR 3.44, 95%CI 1.27-9.33), younger age (OR 0.66 per 10 years, 95%CI 0.54-0.81), and methotrexate use vs. non-use (OR 2.31, 95%CI 1.12-4.79) were associated with repeat COVID-19 infection (Table 3). Among those with repeat COVID-19 infection, 5 (6.6%) were hospitalized and there were no deaths.
Conclusion: In this first study to examine risk factors and outcomes of repeat COVID-19 infection among SARD patients, we identified rituximab use, methotrexate use, and younger age as potential risk factors for repeat COVID-19. While some of the findings may be due to risk mitigation behavior differences, these factors may be useful to raise awareness of repeat COVID-19 risk for patients and clinicians. Reassuringly, there were no deaths and the hospitalization rate was low among those with repeat COVID-19 infection.
To cite this abstract in AMA style:
Kowalski E, Wang X, Patel N, Kawano Y, Cook C, Vanni K, Qian G, Bade K, Srivatsan S, Williams Z, Wallace Z, Sparks J. Risk Factors and Outcomes for Repeat COVID-19 Infection Among Patients with Systemic Autoimmune Rheumatic Diseases: A Case-control Study [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/risk-factors-and-outcomes-for-repeat-covid-19-infection-among-patients-with-systemic-autoimmune-rheumatic-diseases-a-case-control-study/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/risk-factors-and-outcomes-for-repeat-covid-19-infection-among-patients-with-systemic-autoimmune-rheumatic-diseases-a-case-control-study/