Session Information
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Recent studies have suggested that right ventricular (RV) adaptation in patients with scleroderma-associated pulmonary arterial hypertension (SSc-PAH) is worse than in patients with idiopathic pulmonary arterial hypertension (IPAH). This has been proposed as one of the explanations for increased mortality in SSc-PAH. However, few studies have compared incident groups of treatment naive SSc-PAH and IPAH patients. The objective of this study is to compare RV remodeling and load-adaptability metrics in patients with SSc-PAH versus IPAH at the time of diagnostic right heart catheterization (RHC) at our institution and at 1 year follow up.
Methods: A retrospective review of adults with SSc-PAH and IPAH who underwent RHC at Stanford Medical Center between 2002-2016 was performed. Inclusion criteria were as follows: mean pulmonary artery pressure (mPAP) greater than or equal to 25 mmHg, baseline echocardiogram within 3 months of RHC, absence of left heart disease (pulmonary capillary wedge pressure less than or equal to 15 mmHg), and absence of severe ILD (FVC and/or TLC < 70%). Baseline characteristics, RHC parameters, and standard echocardiographic measurements including right ventricular fractional area change (RVFAC), tricuspid annular plane systolic excursion (TAPSE), and RV global longitudinal strain (RV GLS) were obtained. Load-adaptability metrics, including the ratio of cardiac index to mean pulmonary artery pressure (CI/mPAP), right atrial pressure to pulmonary pulse pressure (RAP/PP), and RV global longitudinal strain to pulmonary vascular resistance (RV GLS/PVR) were compared between the SSc-PAH and IPAH groups. We used non-parametric Mann Whitney U-test for continuous variables and Fischers Exact Test for categorical variables. Change in RV function was examined by follow up echo (1 year post-RHC) in a subset of patients matched on PH-directed therapy.
Results: Twenty-four PVR matched SSc-PAH and IPAH subjects with newly diagnosed PAH were included in the study. Average duration of SSc was 3 years and median PVR was 12 (3-25 Wood units). There was no significant difference between the two groups in age, sex, baseline NT-proBNP, or degree of treatment at 1 year. At baseline there was no difference in resting right ventricular metrics, including RV FAC, RV GLS, TAPSE, or right atrial size (Table 1). With regards to load-adaptability, there was no difference in RAP/PP, CI/MPAP, or the RV load-adaptability metrics allometrically adjusted for PVR in each group. Overall there was improvement in RVFAC, RV GLS, and TAPSE at 1 year in both groups, though notably we did not observe a significant difference in the degree of response in RV function to therapy between Ssc-PAH and IPAH.
Conclusion: In well-matched SSc-PAH and IPAH patients without ILD or left heart disease, we did not observe a difference in baseline RV function or response to treatment. 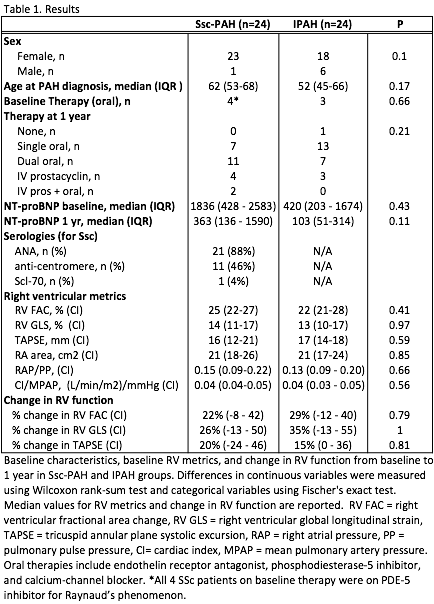
To cite this abstract in AMA style:
French S, Ouazani N, Amsallem M, Li S, Zamanian RT, Chung L, Haddad F. Right Ventricular Load-Adaptability and Response to Therapy in Scleroderma Versus Idiopathic Pulmonary Arterial Hypertension [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/right-ventricular-load-adaptability-and-response-to-therapy-in-scleroderma-versus-idiopathic-pulmonary-arterial-hypertension/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/right-ventricular-load-adaptability-and-response-to-therapy-in-scleroderma-versus-idiopathic-pulmonary-arterial-hypertension/
