Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Rheumatic disease patients are counseled on the immunosuppressive aspect of their rheumatic disease treatment and their increased risk of infection. Little is known about the experience of rheumatic disease patients during a pandemic, their medication trends, or resource utilization.
Methods: Rheumatologist-created 32 question electronic questionnaire was shared through social media platforms including Facebook, Reddit, and Twitter on disease-specific pages from April-June 2020 with goal of being by patients with any rheumatic disease.
Results: 2244 questionnaires were completed, the majority by Caucasian women (88%) ages 35-64 from across the United States (85%) who had obtained higher education. Multiple self-declared diagnoses could be chosen, the majority had any form of inflammatory arthritis (59%) with systemic lupus, mixed connective tissue disease, and Sjogren’s syndrome noted by 23%. All categories of rheumatic diseases were represented. Most commonly used medications were: Corticosteroids, TNF inhibitors, NSAIDs, and Methotrexate, 5% were on no medications (Figure 1). One quarter of subjects had a pulmonary, renal, and/or cardiac condition. Eighty percent of those surveyed considered themselves immunocompromised, with 4% of these on no immunosuppressive medications. When typically ill almost half of patients reported they continue all of their medications.
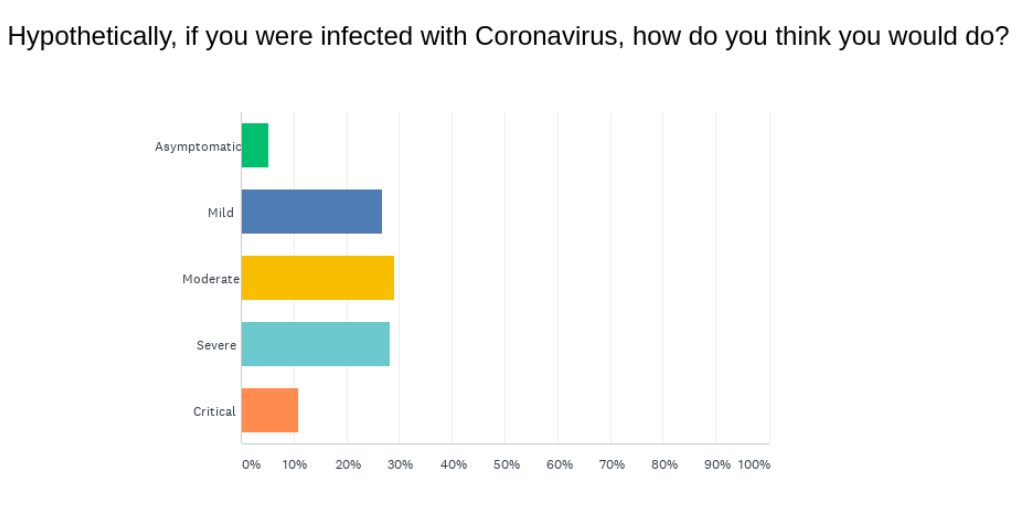
Across all diseases, almost 50% had contacted their rheumatologist or another medical provider with questions regarding the novel coronavirus in the past 8 weeks prior to the survey completion, with those on no medications more likely to reach out. In this time period, 20% held at least one of their medications. Of those, 15% held their rheumatic medication as directed by their rheumatologist due to the SARS-Cov-2 pandemic (not infected) and 30% held medication without medical consultation. Specifically 10% stopped taking NSAIDs due to concern of SARS-CoV-2. Patients felt they would do poorly if infected with SARS-CoV-2 (Figure 2) this correlated with underlying pulmonary, renal, or cardiac conditions but also correlated with the patient reported taking no medications. Medications popularized at time of survey with potential to treat SARS-CoV-2 were not correlated with presumption of less severe outcomes.
Very few had been diagnosed with SARS-CoV-2 (0.7% tested, 3% presumed), nor had their household contacts. Only about 40% were working from home, 12% of those surveyed were unemployed or furloughed. Traditional news sources was the most often consulted resource as knowledge in regard to how coronavirus affects those with rheumatic diseases, followed by disease-specific foundations and the CDC.
Conclusion: In the initial months of the SARS- CoV-2 pandemic, patients were either told to stop or self-stopped their rheumatic disease medications. Patients overall felt they would do worse than those without a rheumatic disease, however did not correlate to specific medication or disease but with organ involvement. Disease specific foundations were seen as a resource for reliable information pertaining to their disease.
To cite this abstract in AMA style:
Edens C, Ko K, Trotter K. Rheumatology Patient Experience and Trends During the SARS-COV-2 Pandemic [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/rheumatology-patient-experience-and-trends-during-the-sars-cov-2-pandemic/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/rheumatology-patient-experience-and-trends-during-the-sars-cov-2-pandemic/