Session Information
Session Type: Poster Session C
Session Time: 1:00PM-3:00PM
Background/Purpose: To investigate (1) agreement between local and central reading of sacroiliac joint images (X-ray and magnetic resonance imaging [MRI]) from axial spondylarthritis (axSpA) patients, and (2) to explore potential differences between patients diagnosed in an academic hospital compared to community centres.
Methods: The BelGian Inflammatory Arthritis and spoNdylitis cohort (Be-GIANT) includes newly diagnosed biological-naïve axSpA patients, that fulfil the ASAS classification criteria, at the outpatient clinic of an academic hospital and eight community centres in Flanders. X-ray and MRI of the sacroiliac joints (SIJ) of patients enrolled between November 2010 and August 2020 were assessed by the local rheumatologist (‘local reading’) and two calibrated central readers (‘central reading’) for definite radiographic sacroiliitis according to the modified New York criteria (X-SIJ) and active sacroiliitis according to the ASAS/OMERACT definition of a positive MRI (MRI-SIJ). Central readers resolved discrepant cases by consensus. Inter-reader reliability was assessed with Cohen’s Kappa, and % overall, positive and negative agreement.
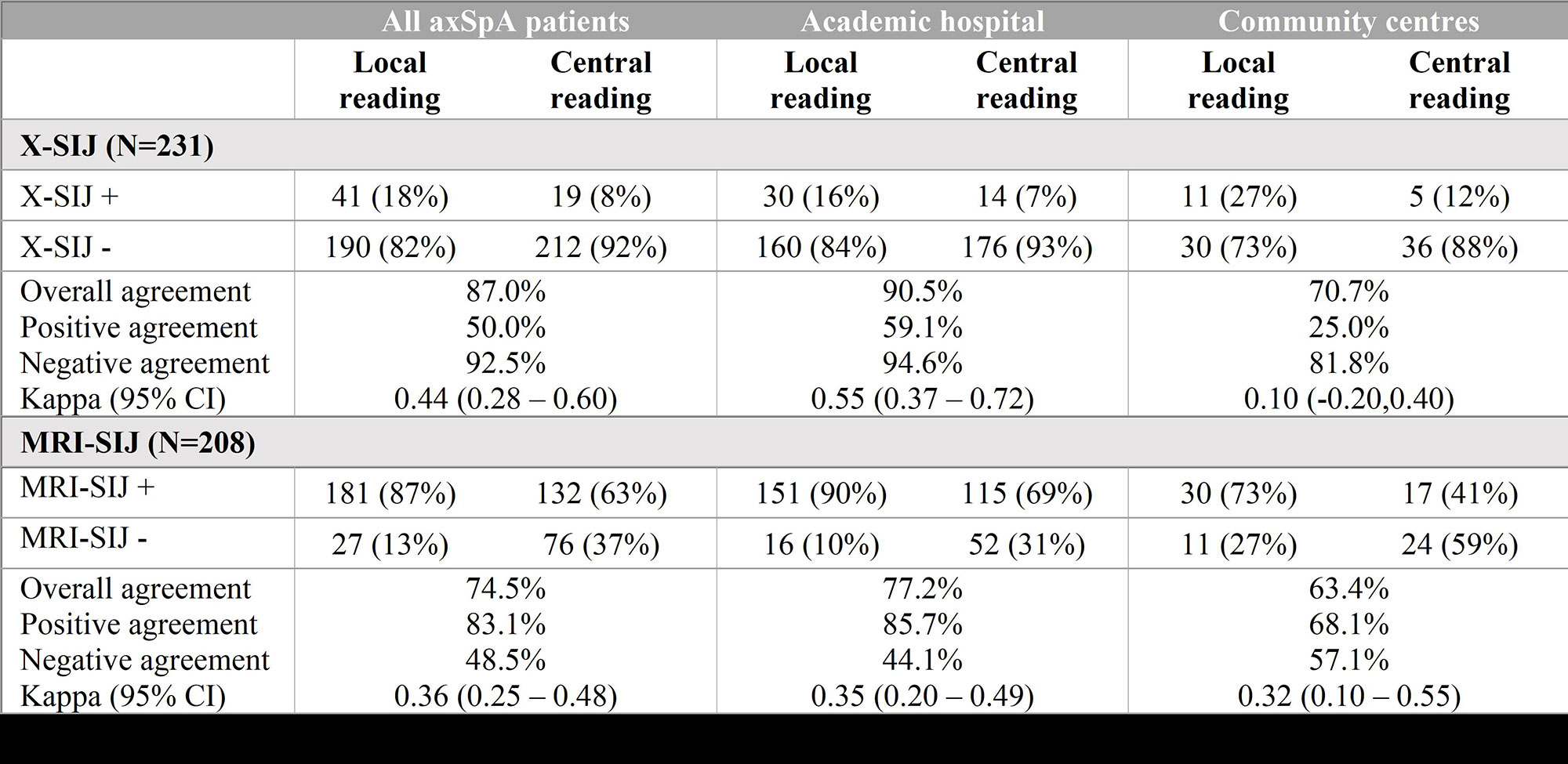
Results: Among the 271 included patients (n=205 academic hospital, n=66 community hospital), 231 X-SIJ and 208 MRI-SIJ were available for central reading (Table 1). Central readers disagreed with local readers on 30/231 (13%) X-SIJ images (κ=0.44, moderate); 4/231 (1.7%) were reclassified as radiographic sacroiliitis and 26/231 (11.3%) as not showing radiographic sacroiliitis. Overall agreement was higher between central readers and academic rheumatologists compared to community rheumatologists (90.5% vs. 70.7%, p< 0.001). 53/208 (25.4%) MRI-SIJ images were reclassified by central readers (κ=0.36, fair); the majority as negative for active sacroiliitis (51/208, 24.5%). Central readers agreed on the assessment of MRI-SIJ in a higher proportion with academic rheumatologists versus community rheumatologists (77.2% vs. 63.4%, p=0.07).
Conclusion: In newly diagnosed axSpA patients, the prevalence of radiographic sacroiliitis is low. Sacroiliitis on MRI is overcalled by rheumatologists both in academic and non-academic settings, leaving opportunities for educational interventions.
To cite this abstract in AMA style:
De Craemer A, de Hooge M, Renson T, Deroo L, Varkas G, Van Praet L, Joos R, Lenaerts J, Devinck M, Gyselbrecht L, peene i, Thevissen K, Carron P, Van den bosch F, Elewaut D. Rheumatologists Overcall Sacroiliitis on X-ray and MRI in Axial Spondyloarthritis Patients: Data from the BelGian Inflammatory Arthritis and SpoNdylitis cohorT (Be-GIANT) [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/rheumatologists-overcall-sacroiliitis-on-x-ray-and-mri-in-axial-spondyloarthritis-patients-data-from-the-belgian-inflammatory-arthritis-and-spondylitis-cohort-be-giant/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/rheumatologists-overcall-sacroiliitis-on-x-ray-and-mri-in-axial-spondyloarthritis-patients-data-from-the-belgian-inflammatory-arthritis-and-spondylitis-cohort-be-giant/