Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Patients with a chronic inflammatory disease (CID), particularly rheumatoid arthritis (RA), have an increased risk of fatal myocardial infarction (MI), as compared to the general population. This risk might be explained, in part, by an increased systemic inflammatory burden in CID causing coronary plaque instability. With tissue specimens of epicardial coronary arteries, we studied whether individuals with CID who died of a fatal MI have an increased influx of inflammatory cells, as compared to individuals without CID but with fatal MI.
Methods: All epicardial coronary artery tissue was collected from 11 individuals with CID (including RA) who had a fatal MI and controls without CID who also had a fatal MI. Controls were matched for age, gender and maximum stenosis of coronaries. Coronary arteries were immunohistochemically stained with specific antibodies against myeloperoxidase (neutrophilic granulocytes), CD45 (lymphocytes), CD68 (macrophages) and tryptase (mast-cells). Intramyocardial coronaries were stained with N-epsilon-(Carboxymethyl)lysine (CML), an advanced glycation end product, visualizing a pro-inflammatory status. Inflammatory cell density (cells/mm2) was calculated for each section of the coronary artery (intima, media and adventitia) for each stain. Subsequently, grade of coronary stenosis (0-100%) was measured. Correlations of grade of coronary stenosis and inflammatory cell density within each of these groups was calculated using the non-parametric Spearman’s Rank correlation.
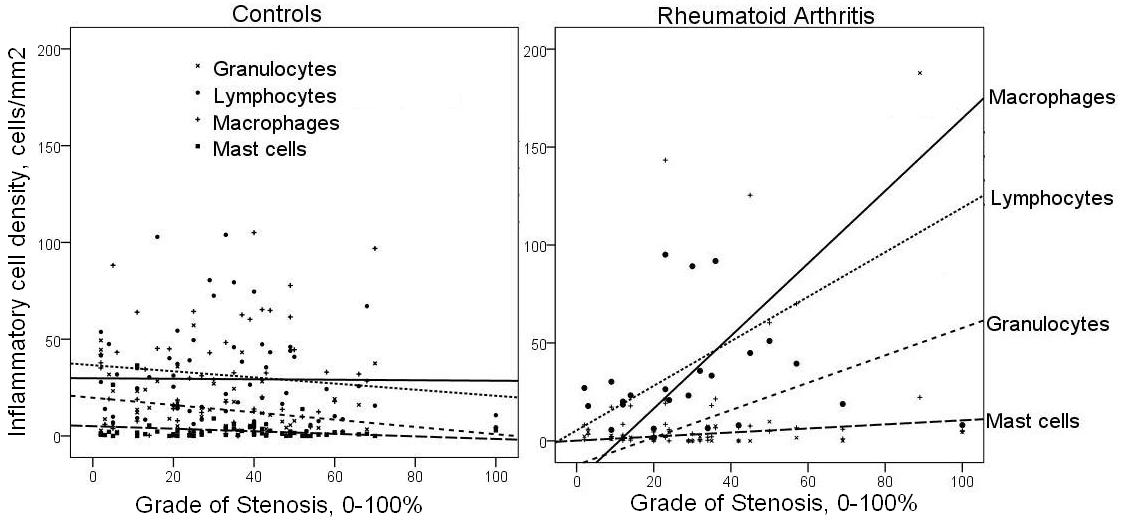
Results: In RA patients, there was a significant correlation between grade of stenosis and inflammatory cell density of macrophages and lymphocytes in the intima of coronaries , with correlation coefficients of 0.313 (p < 0.05) and 0.205 (p < 0.05), respectively. This was also noted in granulocyte and mast-cell staining, but less strongly. These correlations were not observed in the control group and were also not observed in the media or adventitia of coronaries. Also, in patients with RA, a pro-inflammatory status of intramyocardial coronaries was shown, not only around the infarcted areas, but also in areas of the myocardium distant from MI.
Conclusion: Patients with RA who developed a fatal MI had a significant association between increasing grade of coronary stenosis and influx of inflammatory cells into the intima of all coronary arteries, irrespective of their relationship with the coronary implicated in MI. In particular, an increased influx of macrophages and lymphocytes was noted in the intima of all epicardial coronaries, as well as an increased endothelial activation of intramyocardial coronary vessels. The underlying inflammatory process in RA might drive a more inflammatory form of atherosclerosis, resulting in plaque vulnerability.
Figure 1. Scatter-plot depicting the correlation between inflammatory cell density of the intima and grade of stenosis of the epicardial coronary
Disclosure:
I. A. M. van den Oever,
None;
A. M. van Sijl,
None;
U. Baylan,
None;
M. T. Nurmohamed,
None;
A. E. Voskuyl,
Actelion Pharmaceuticals,
5;
H. W. Niessen,
None;
S. Simsek,
None.
« Back to 2013 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/rheumatoid-arthritis-is-associated-with-systemic-inflammation-in-coronary-vessels/