Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: For rheumatoid arthritis (RA) American College of Rheumatology (ACR) recommends the treating to target approach, starting with conventional synthetic antirheumatic drugs (DMARDs). ACR advises as many switches as necessary to achieve the target. Patients may switch therapy because of adverse reactions, response failure, or non-medical (e.g., economic) reasons. Prior research has reported that treatment switching is associated with increased healthcare burden and costs, however a summary of the published literature is lacking. We aimed to summarize published literature reporting clinical and economic burden of treatment switching in RA.
Methods: We used PubMed and desktop search to identify literature reporting healthcare resource use (HCRU) or costs associated with treatment switching in RA patients. Keywords: RA AND treatment switch* AND [HCRU OR cost].
Results: The PubMed search yielded 100 titles; 48 were selected for abstract review, 16 selected for full-text review (8 articles excluded as not relevant). Three articles were identified via desktop search.
Eleven articles reported research conducted in USA (n=9; commercial claims), Sweden (n=1), and Italy (n=1). Nine articles reported results for RA only; two reported RA within a mix of inflammatory conditions. Outcomes were for patients who switched therapy after initiating oral methotrexate (n=1), first biologic DMARD (n=5), biologic DMARD (n=4), or first targeted DMARD (biologic or JAKi; n=1).
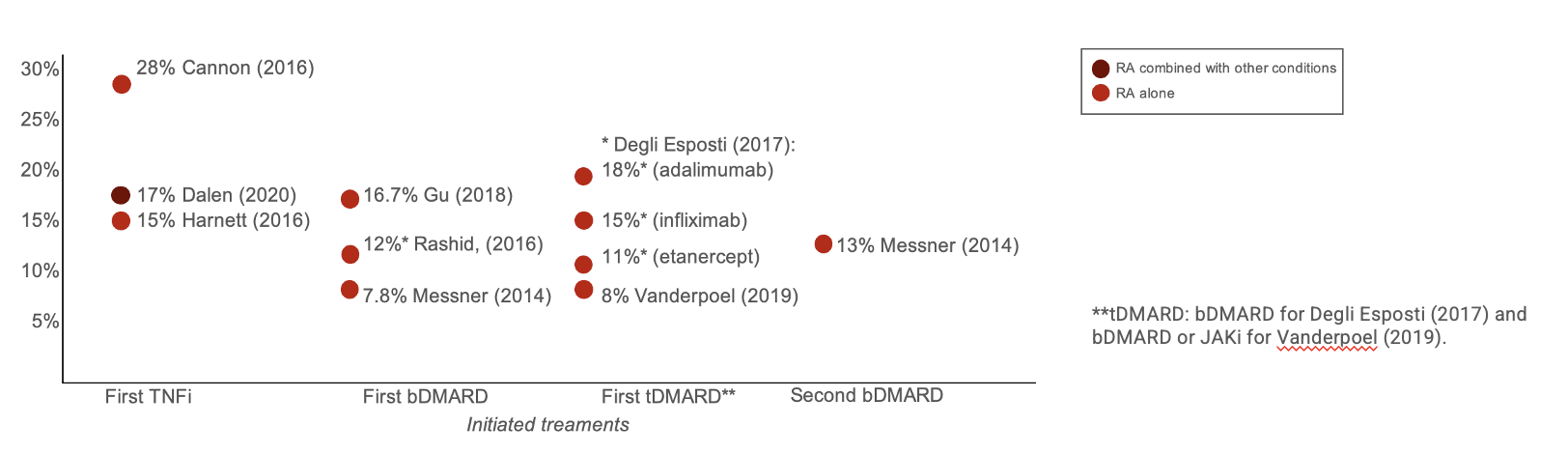
After treatment initiation, treatment switch was reported in 12%-18% patients (8% in one study) within 1 year and 30% within 2 years (Figure 1). Treatment switching was associated with 5%-51% increase in adjusted all-cause healthcare costs (Figure 2). One study (Vanderpoel, et. al., 2019) reported switching to be associated with increased adjusted HCRU: hospitalization (adjusted odds ratio [aOR]: 3.03; P< 0.05), emergency department use (aOR: 1.73, P: NS), and outpatient visits (aOR: 1.05, P: NS).
Within studies, risks of bias included: reporting of unadjusted estimates (failing to account for between-group differences; n=3), combining RA with other inflammatory conditions (n=2), combining outcomes [switchers and discontinuers (n=1) and non-switchers into one group (n=5)]. All studies had bias towards reporting data from US commercial databases (all prior to 2016), mostly biologic DMARD; few studies reported HCRU.
Conclusion: Published literature consistently reported frequent therapy switching in RA. The switching was associated with increased HCRU and costs, highlighting the health economic need for prognostic markers of sustained response. Additional research is needed to report contemporary trends, outcomes in Medicare and Medicaid, and trends outside of the US.
References:
Degli Esposti, et. al. (2017); PMID:28053549
Cannon, et. al. (2016); PMID:27352377
Dalen, et. al. (2020); PMID:32647910
Gu, et. al. (2018); PMID:30020745
Harnett, et. al. (2016); PMID:26401963
Rashid,, et. al. (2016); PMID:26766553
Vanderpoel, et. al. (2019); PMID:31122662
Messner, et. al. (2014); PMID:24575891
Wolf, et. al. (2017); PMID:28363696
Lee, et. al. (2017); PMID:28465768
Shahabi, et. al. (2019); PMID:30653389
To cite this abstract in AMA style:
Taylor P, Antonova J. Review of Published Literature Reporting Economic Burden of Treatment Switching in Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/review-of-published-literature-reporting-economic-burden-of-treatment-switching-in-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/review-of-published-literature-reporting-economic-burden-of-treatment-switching-in-rheumatoid-arthritis/