Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: The COVID-19 pandemic has significantly changed the understanding of the safety profile of therapies for immunoinflammatory rheumatic diseases. This is primarily due to the negative impact of a number of DMARDs and biological DMARDs on the course and outcomes of a new coronavirus infection. A number of studies have shown that anti-B-cell therapy (rituximab) was associated with statistically significant increase in the risk of severe COVID-19 and an increase in mortality. At the same time, the analysis of real clinical practice data dictated the need to establish a number of restrictions on the use of certain classes of biological DMARDs and to search for alternative therapeutic approached to maintain control over disease activity.
We evaluate the efficacy and safety of olokizumab, solution for subcutaneous injection, 160mg/ml – 0.4ml for the treatment of patients with RA in real clinical practice after switchingfrom rituximab during the COVID-19 pandemic.
Methods: The study included 19 patients with a confirmed diagnosis of RAwho were previously on rituximab therapy at a dose of 1000 (500) mg twice with an interval of 2 weeks not less than 6 months,and received at least one course of therapy with this drug. As RA worsened, patients switched to olokizumab and continued to receive standard DMARDs. At weeks 0, 4, 8, 12, 16, 20 and 24 after the switch, the following parameters were assessed: the severity of pain(VAS scale), the number of tender and swollen joints (TJC28 and TSC28), the level of acute phase markers of inflammation, the disease activity index (DAS28) calculated using ESR and CRP, and the CDAI (clinical disease activity index), functional state index HAQ, as well as the safety profile of therapy.
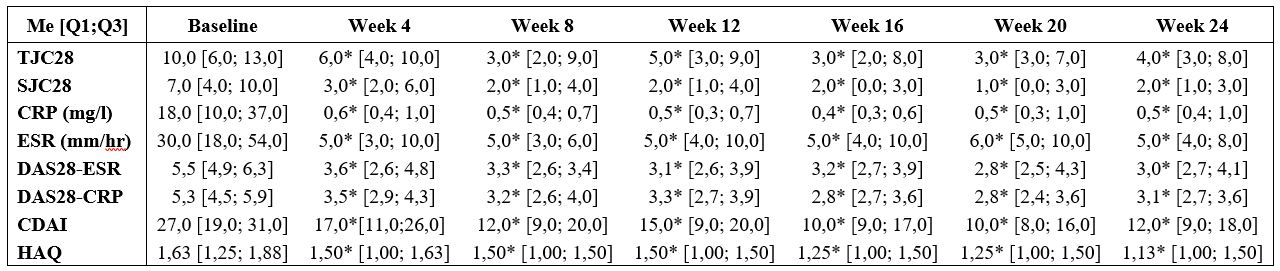
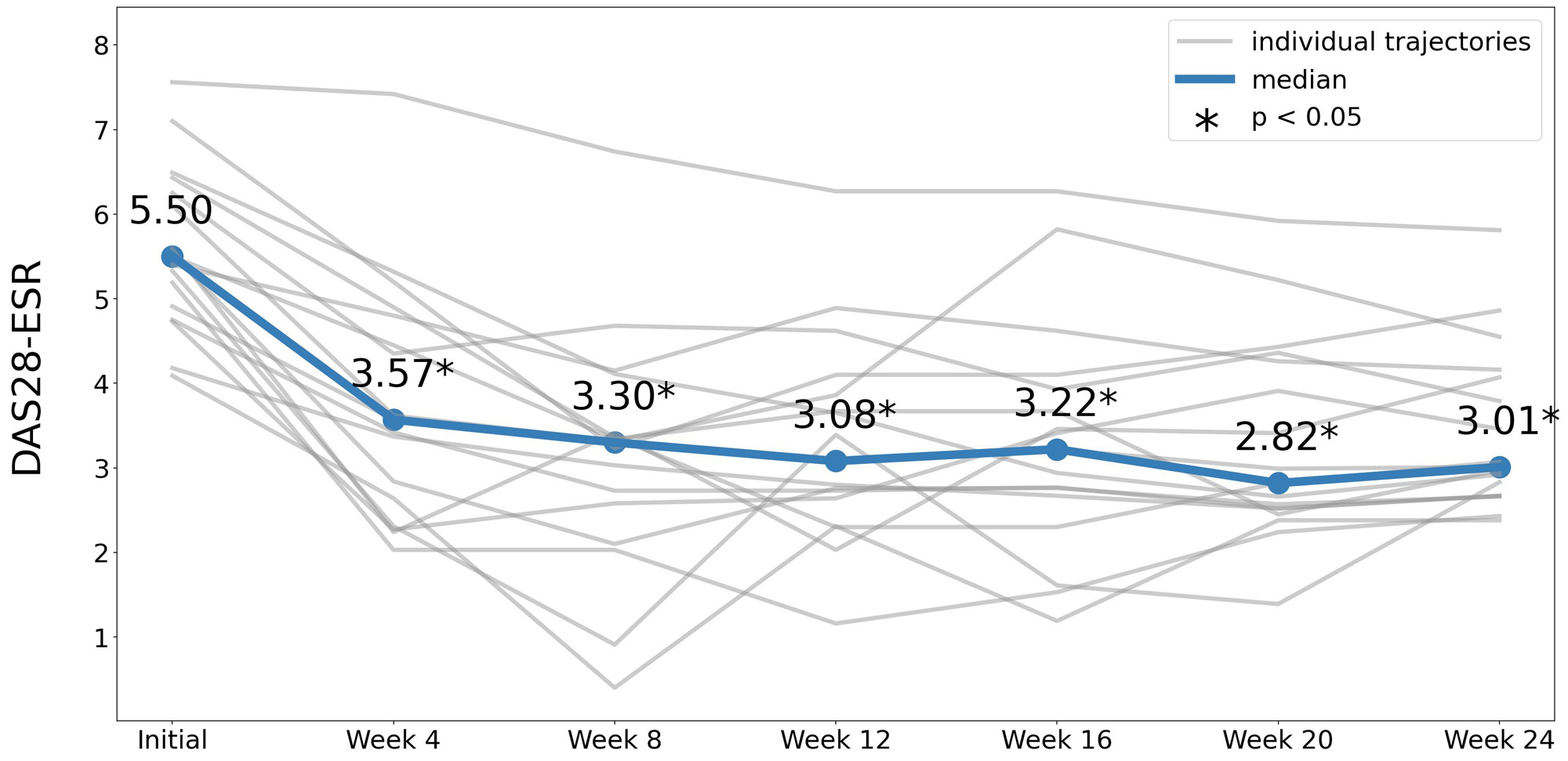
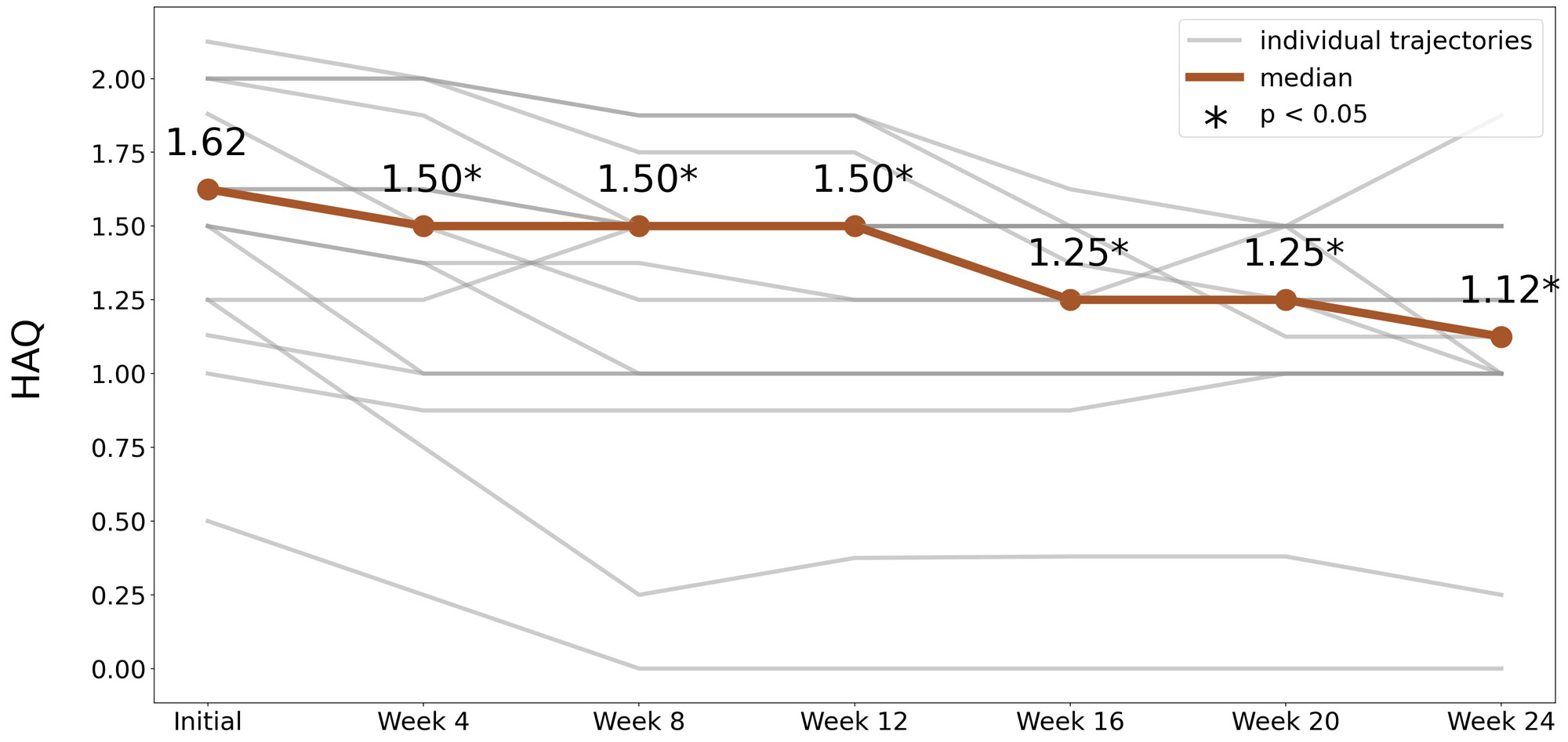
Results: Data analysis was performed using median values (Me). TJC28 and SJC28 decreased 4 weeks after the injection of olokizumab in comparison to baseline values (Table 1). Laboratory markers of inflammation analysis showed a decrease in CRP and ESR levels after 4 weeks of treatment with positive trend in place at weeks 8, 12, 16, 20 and 24. The level of CRP by the week 4 became within the normal range, regardless of the baseline values (Table 1). All activity indices improved from the week 4 in each evaluation period compared to baseline (Table 1, for DAS28-ESR see Figure 1). All patients showed a reduction in pain (VAS scale) improved starting from week 4. There was a significant improvement in the functional status of patients by study week 4 according to the HAQ index (Figure 2).
Conclusion: The study found that non-medical switching from rituximab to olokizumab was effective and safe during the COVID-19 pandemic.
Footnotes: *p<0.05 compared to baseline; Me [Q1;Q3]. median [1st; 3nd quartile]
To cite this abstract in AMA style:
Kuzkina S, Feist E, Banshchikova N, Akimova A, Sizikov A, Mullagaliev A, Ilina N, Letyagina E, Korolev M. Results of a 24-week Open-label, Non-interventional Study of the Efficacy and Safety of Olokizumab Therapy in Patients with Rheumatoid Arthritis After Switching from Anti-B-cell Therapy During the SARS-COV-2 Pandemic [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/results-of-a-24-week-open-label-non-interventional-study-of-the-efficacy-and-safety-of-olokizumab-therapy-in-patients-with-rheumatoid-arthritis-after-switching-from-anti-b-cell-therapy-during-the-sar/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/results-of-a-24-week-open-label-non-interventional-study-of-the-efficacy-and-safety-of-olokizumab-therapy-in-patients-with-rheumatoid-arthritis-after-switching-from-anti-b-cell-therapy-during-the-sar/