Session Information
Session Type: Poster Session D
Session Time: 8:30AM-10:30AM
Background/Purpose: Rheumatoid arthritis (RA) is a systemic inflammatory disease that affects glucose metabolism, mainly insulin resistance, which can lead to diabetes mellitus (DM). Although there have been reports that anti-inflammatory therapy can reduce the risk of diabetes in RA, the relationship between individual antirheumatic drugs and DM has not been sufficiently investigated. Therefore, we aimed to investigate the effect of disease-modifying antirheumatic drugs (DMARDs) on the incidence of DM in the RA population.
Methods: We conducted a nested case-control study in a cohort of 69 779 DM-naïve adult (≥ 18 years old) patients with RA from the Korean Health Insurance Review and Assessment Service claims data from 2011 to 2019. Cases with incident DM were identified and individually matched to randomly selected controls (RA cases without DM) by the age of RA diagnosis, sex, and disease duration (1:4 matched). Comorbidities including hypertension, chronic kidney disease, Charlson Comorbidity Index (CCI), and concomitant drug use were measured for one year prior to the event or index date. DMARDs use was stratified by duration of exposure. The association of each DMARD use with DM risk was estimated using conditional logistic regression adjusted for CCI and concomitant drug use.
Results: 3772 (5.4%) patients were diagnosed with DM (mean age, 62.3 ± 10.9 years; 77,6% women), and the mean duration between RA diagnosis and incident DM was 2.6 ± 2.1 years. A total of 146139 controls were matched, and DM risk was associated with corticosteroids use and cumulative dosage. 3515 of 3772 (93.2%) patients with DM have been treated with conventional DMARDs. The risk of incident DM was dependent on the type and the duration of exposure of DMARDs (Figure). In a multivariable-adjusted analysis, exposure of less than 90 days per year to hydroxychloroquine (HCQ), methotrexate (MTX), sulfasalazine, leflunomide, tacrolimus (TAC), or any targeted synthetic DMARDs (tsDMARDs) was associated with an increased risk of DM compared with no use. However, at exposure exceeding 270 days per year, HCQ (adjusted OR, 0.76; 95% CI, 0.69-0.84; p < 0.001) and MTX (adjusted OR, 0.81; 95% CI, 0.74-0.89; p < 0.001) were associated with a significant decrease in DM risk, and TAC (adjusted OR, 1.27; 95% CI, 1.07-1.51; p = 0.006) was associated with an increased risk. Among biologic DMARDs, use of TNF inhibitors or non-TNF inhibitors was not related to DM risk at exposure less than 90 days per year, but non-TNF inhibitors was associated with a significant decrease in DM risk at exposure more than 270 days per year (adjusted OR, 0.52; 95% CI, 0.29-0.93, p = 0.026).
Conclusion: This study suggested that long-term use of HCQ, MTX, or non-TNF inhibitors for periods more than 270 days per year was associated with a reduction in the incidence of DM. Thus, these regimens could be considered to control disease activity especially in patients with high risk of DM.
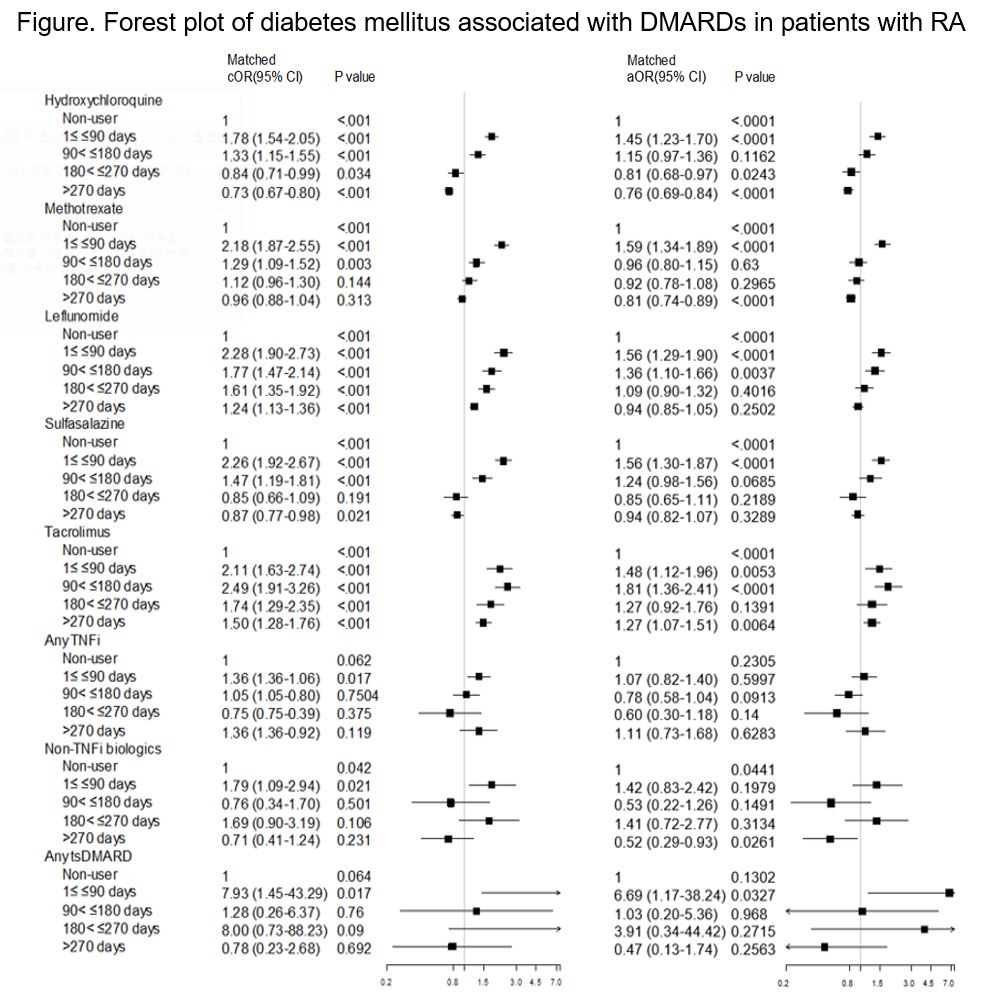 Abbreviations: DMARDs, disease-modifying anti-rheumatic drugs; RA, rheumatoid arthritis; OR, odds ratio; CI, confidence interval; TNFi, tumor necrosis factor inhibitor; tsDMARDs, targeted synthetic disease-modifying anti-rheumatic drugs; CCI, Charlson Comorbidity Index. Adjusted for CCI (ordinal), use of steroid (cumulative prescribed dose quintiles), use of statin (yes/no), use of other DMARDs, or use of TNFi
Abbreviations: DMARDs, disease-modifying anti-rheumatic drugs; RA, rheumatoid arthritis; OR, odds ratio; CI, confidence interval; TNFi, tumor necrosis factor inhibitor; tsDMARDs, targeted synthetic disease-modifying anti-rheumatic drugs; CCI, Charlson Comorbidity Index. Adjusted for CCI (ordinal), use of steroid (cumulative prescribed dose quintiles), use of statin (yes/no), use of other DMARDs, or use of TNFi
To cite this abstract in AMA style:
Nam S, Kim M, kim Y, Ahn S, Hong S, Lee C, Yoo B, Oh J, Kim Y. Relationship Between Risk of New Onset Diabetes Mellitus and Exposure to Individual Antirheumatic Drugs in Patients with Rheumatoid Arthritis: A Nationwide Population Study [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/relationship-between-risk-of-new-onset-diabetes-mellitus-and-exposure-to-individual-antirheumatic-drugs-in-patients-with-rheumatoid-arthritis-a-nationwide-population-study/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/relationship-between-risk-of-new-onset-diabetes-mellitus-and-exposure-to-individual-antirheumatic-drugs-in-patients-with-rheumatoid-arthritis-a-nationwide-population-study/
