Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: The pain experience in osteoarthritis (OA) is multifactorial and includes both somatosensory and affective components. The affective component can be related to depression, a common comorbidity in OA. Some antidepressants such as tricyclic antidepressants (TCA) (e.g., amitriptyline) and serotonin-norepinephrine reuptake inhibitors (SNRI) (e.g., duloxetine) have been reported to alleviate pain. Anticonvulsants such as gabapentinoids (GBP) are also used for pain management and off-label for depression. While selective serotonin reuptake inhibitors (SSRI) such as fluoxetine are used primarily for their antidepressant effects, whether they have pain relieving effects is less clear. We aimed to evaluate the relation of analgesic antidepressants (AAD: TCA, SNRI, and GBP) compared with SSRIs to measures of pain severity and pain sensitization in knee OA.
Methods: We included participants from the Multicenter Osteoarthritis (MOST) Study, a NIH-funded longitudinal cohort of older adults with or at risk of knee OA, who used AAD and/or SSRI and also had radiographic OA (ROA) (KL grade ≥2) in at least one knee. We characterized participants as being on AAD only, SSRIs only, or both at baseline. We assessed knee pain severity using WOMAC pain at baseline and two years later. We used quantitative sensory testing (QST) to measure pain sensitization (pressure pain threshold (PPT) at the patella and wrist, temporal summation (TS)) and descending modulation (conditioned pain modulation (CPM)) at baseline and two years later. We evaluated the relation of AAD (with or without SSRIs) compared with SSRI use alone to pain and QST measures cross-sectionally and longitudinally in knee-based analyses using linear or logistic regression as appropriate with generalized estimating equations (GEE) to account for correlation between two knees, adjusted for potential confounders.
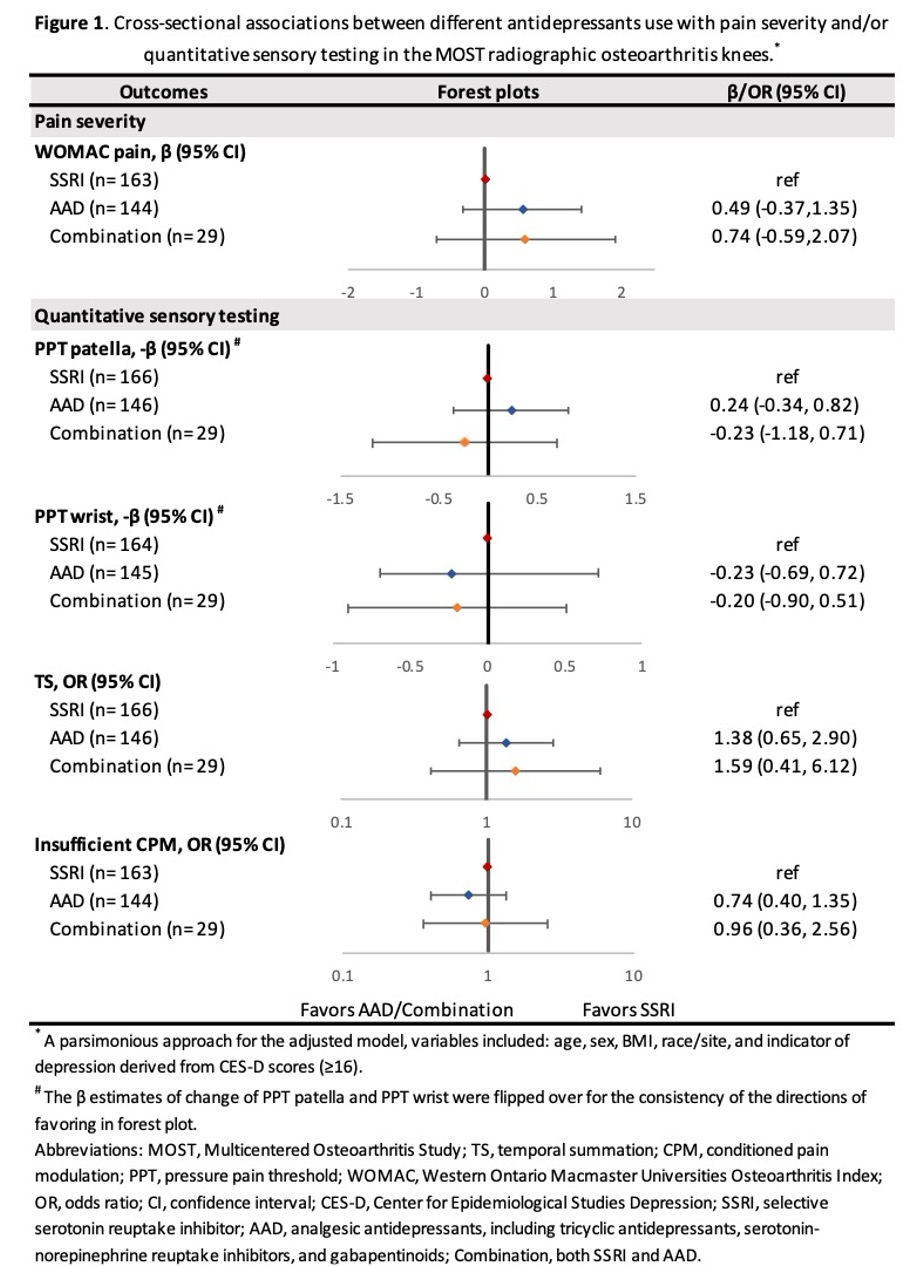
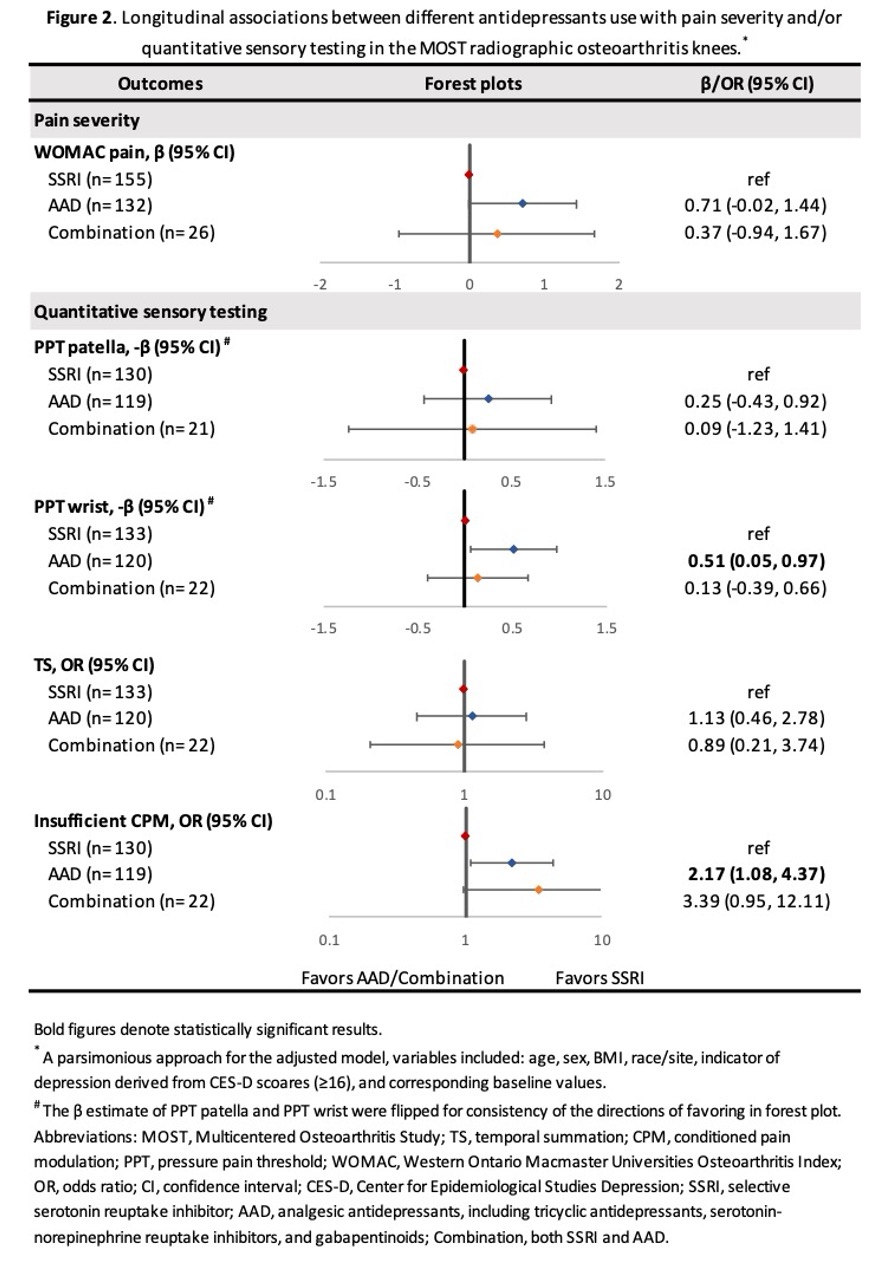
Results: We included 224 participants (mean age 67.6 years, female 75.5%, and mean BMI 31.6 kg/m2), in whom 342 of their knees had ROA (146 in the AAD group, 166 knees in the SSRI group, and 30 in the combination group). Cross-sectionally, there was no association between the drug classes with WOMAC pain, nor with any of the QST measures. Longitudinally, AAD users had marginally greater pain two years later compared to SSRI users (β, 95% CI: 0.71 [-0.02, 1.44]). AAD users also had lower PPT at the wrist two years later (β, 95% CI: 0.51 [0.05, 0.97]), and were more likely to have insufficient CPM (OR, 95% CI: 2.17 [1.08, 4.37]), compared to SSRI users, but there were no significant differences in PPT at the patella or TS (Figure 2).
Conclusion: AAD users appear to have more pain severity and worse pain sensitization measures compared to SSRI users related to inadequate descending modulation (CPM) and possibly central sensitization (wrist PPT, but not TS). Whether these effects are reflective of confounding by indication or effects through depression is unclear. Nonetheless, these results may suggest that managing depressive symptoms is important for pain management in OA. Our results highlight the important and complex interplay between depression, pain severity, and pain sensitization in people with knee OA.
To cite this abstract in AMA style:
Wang Z, Mcginley B, LaValley m, Frey-Law L, Lewis B, Nevitt M, Clancy M, Ding C, Neogi T. Relation of Different Types of Antidepressants Use to Pain Severity and Measures of Pain Sensitization in Kneeosteoarthritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/relation-of-different-types-of-antidepressants-use-to-pain-severity-and-measures-of-pain-sensitization-in-kneeosteoarthritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/relation-of-different-types-of-antidepressants-use-to-pain-severity-and-measures-of-pain-sensitization-in-kneeosteoarthritis/