Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Despite the increasing number of available targeted therapies (TT) in rheumatoid arthritis (RA), a proportion of RA patients fail to respond to their first TT, and response decreases with increasing TTs exposures. The definition of refractory RA (refRA) patients is complex; however, recent EULAR guidance defines “difficult-to-treat RA” (D2T RA) as a failure of two or more TTs with differing mechanisms of action (TTDMA) with signs suggestive of active disease, and the management of signs and/or symptoms is perceived as difficult by the rheumatologist and/or the patient.
We aimed to determine the clinical and therapeutic profile of refRA, to describe the patterns of drug sequencing in terms of loss of response, non-response or adverse effects that are associated with RefRA.
Methods: Observational retrospective study with a single-center cohort of RA patients (ACR/EULAR 2010 criteria) exposed to TT since 2000 was performed. We defined refRA as failure of at least 2 TTDMA with moderate/high activity at the TT onset. Demographic and clinical variables were extracted from the electronic medical record, and we analyzed the different lines of treatment with TTs, its duration treatment and reasons for treatment discontinuation.
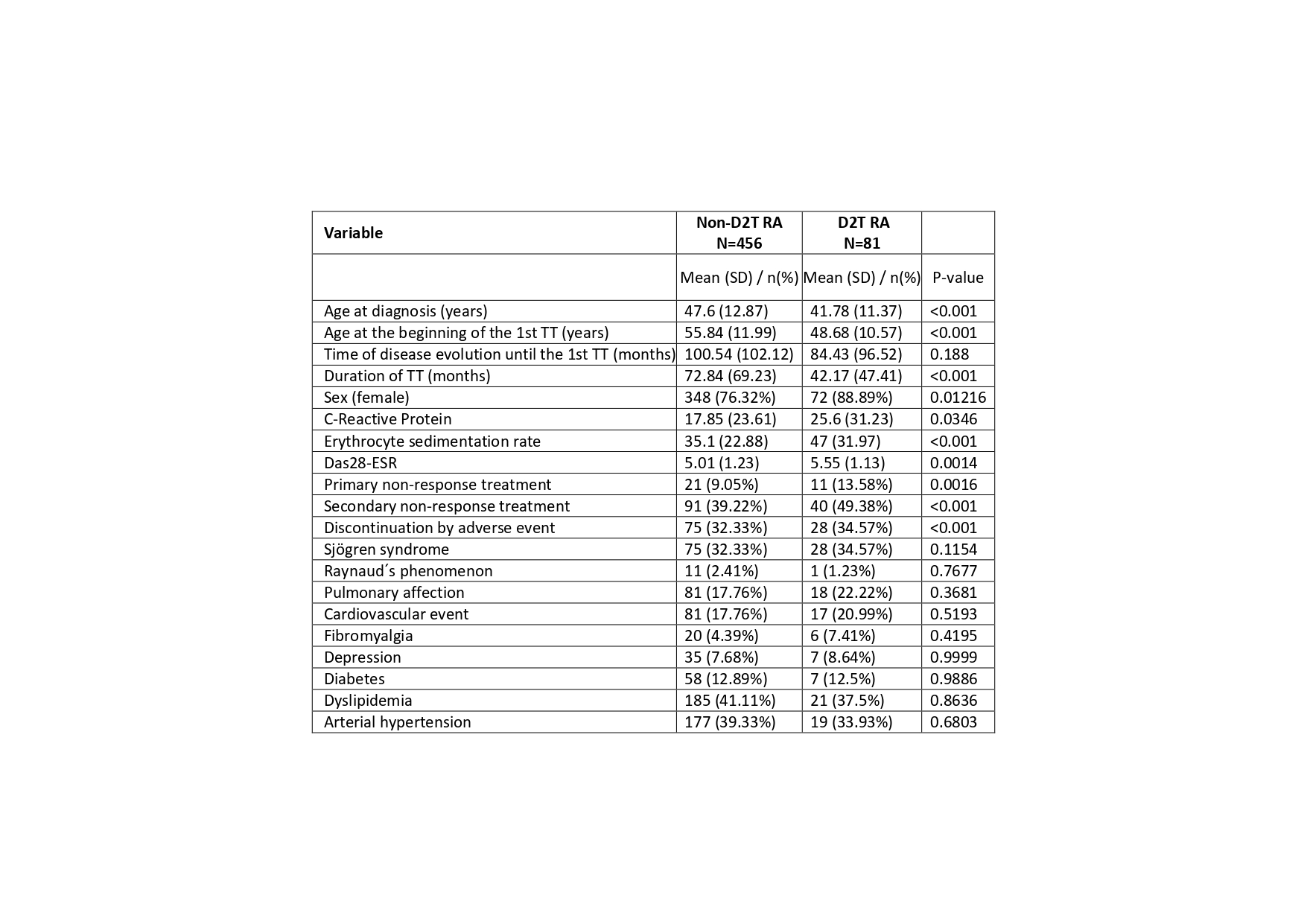
Results: 537 RA patients undergoing TTs were included, 81 from them were considered as refRA. Clinical and demographic characteristics are listed in table 1.
In a multivariate logistic regression analysis RefRA patients showed younger age at diagnosis, higher proportion of female sex and Sjögren Syndrome, and higher Das28-ESR values than non-refRA (P< 0.001). No differences in CRP and ESR levels, rheumatoid factor or anti-CCP positivity, cardiovascular events, depression, fibromyalgia or pulmonary affection were observed. A Kapplan-Meier survival analysis showed a shorter length of TT in RefRA than non-RefRA (P< 0.0001).
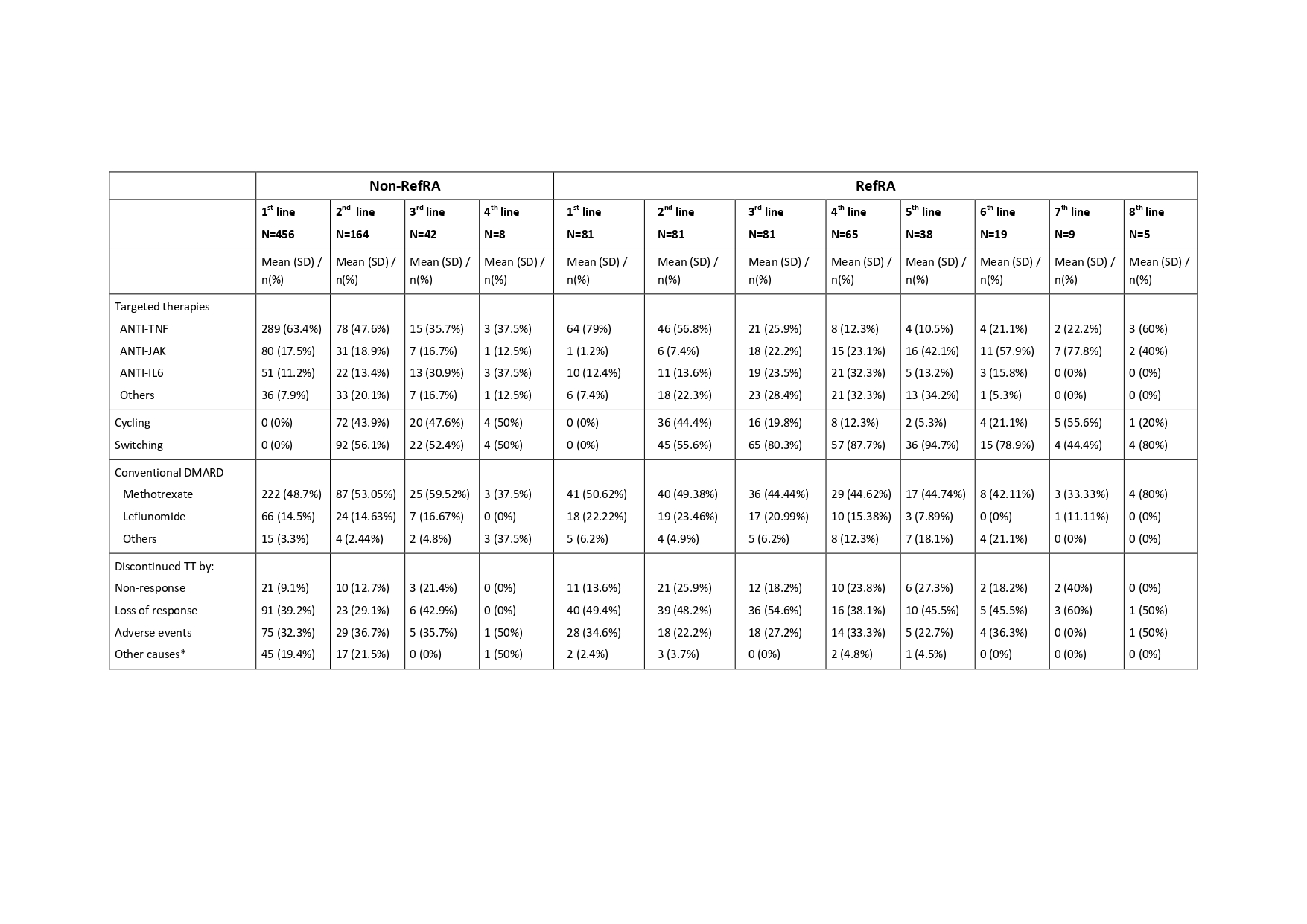
Anti-TNF was the treatment of choice for the 1sr and 2nd TTs, however is less likely to be administered in non-RefRA rather than RefRA (P< 0.001) (table 2), and RefRA showed more incidence of switches (P< 0.001). The absence of conventional DMARD treatment is more likely in Non-RefRA (P=0.046).
Loss of response in 1sr and 2nd TTs were the main reason for discontinuing treatment in refRA, being the adverse event and other causes no related to TT the more frequent as cause of discontinuing TT in non-refRA (P=0.006). When we analyze the reason for discontinuing treatment and excluding the “other causes”, if the cause of discontinuing treatment in refRA is a primary non-response, near of the 30% of patients discontinue in second-line by the same reason; and if the cause for discontinuation in first-line is an adverse effect, the 33% of patients discontinue in second-line by the same reason.
Conclusion: RefRA patients in this study showed lower age at diagnosis, higher proportion of female sex and Sjögren Syndrome. With an exposition of 4 TTs as an average in refRA, the duration of TT is shorter and anti-TNF was the most frequent TT both in first and second line of treatment with more incidence of switching. Loss of response is the most common cause of discontinuation in refRA, with lower rate of adverse events and other causes of discontinuation than non-RefRA.
To cite this abstract in AMA style:
Grau Garcia E, Mas Sanchez L, Muñoz Martínez P, Riesco Barcena C, Torrat Noves A, Ramos Castro D, Huaylla Quispe A, Alcantara Alvarez I, Villanueva Mañez B, Tovar Sugrañes E, Vicens Bernabeu E, Charia H, De la Rubia Navarro M, Gonzalez Puig L, Ivorra Cortes J, Leal Rodriguez S, Martinez Cordellat I, Negueroles Albuixech R, Oller Rodriguez J, Canovas Olmos I, Najera Herranz C, Roman Ivorra J. Refractory RA Patients for Targeted Therapies in Real Life [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/refractory-ra-patients-for-targeted-therapies-in-real-life/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/refractory-ra-patients-for-targeted-therapies-in-real-life/