Session Information
Session Type: Abstract Session
Session Time: 12:00PM-12:50PM
Background/Purpose: Biologic medications are commonly used for numerous rheumatologic conditions. A significant proportion of these medications are denied for non-medical reasons by insurance companies causing delays in patients getting medication which can have negative downstream effects. The aim of this project was to develop an intervention to decrease delays and subsequent associated costs in the approval process of biologics denied for non-medical reasons in rheumatology clinic. Furthermore, we aim to have a 25% usage rate of our intervention by October 1st, 2020.
Methods: To prescribe a biologic in rheumatology clinic, providers fill out a specialty pharmacy (SP) referral through our electronic medical record. They select which medication they would like to use and indication (Figure 1a). This is then sent to our pharmacy department for further review. We assembled a multidisciplinary team of pharmacy, medicine and rheumatology personnel and created a process map of the SP referral process and identified several causes of delay (Figure 2). The longest delay identified was waiting for provider approval of the subsequent, preferred, medication. We recorded the amount of time each step of the process took and their associated costs. We used Kaplan and Porter’s time-driven activity-based costing (Harv Bus Rev, 2011, 89(9), 46-52) to estimate the resulting cost of this process.
Our intervention modified the SP referral to give the ordering physician the ability to allow the pharmacist to switch within the same class of biologic medication if the initial medication is denied (Figure 1b). This extra prompt was created for TNF-α, IL-6, IL-1 and IL-17A inhibitors.
Results: Pre-intervention, we found that 25% of rheumatologic SP referrals at our institution were denied by insurance. On 10/21/2019, our intervention was implemented. Subsequently, we analyzed all SP referrals between 10/21/2019-5/4/2020 and found 210 that were eligible for the ordering provider to use our intervention. The usage rate of our intervention was 15.7% (33/210 referrals). Of these 33 referrals, 21(64%), 7 (21%), and 5 (15%) were for TNF-α, IL-6 and IL-17A inhibitors, respectively. Four (12.1%) were denied by insurance and were appropriately switched to a same-class replacement. Three of these four referrals were for TNF-α inhibitors—the remaining referral was for an IL-17A inhibitor. Notably, the average time between initial referral—including insurance denial—and subsequent approval of the second, insurance-preferred medication, was 19 days post-intervention, compared to an average time of 64 days pre-intervention. Using time-driven activity-based costing, the amount saved each time the intervention was used was estimated to be $42.16.
Conclusion: There is significant time- and cost-related burden when medications are denied for non-medical reasons. Our early results show promise that our intervention will reduce cost and time delays and allow patients to start necessary treatment in a timely fashion. Though close, we have not yet met our desired usage rate but anticipate that we will be able to raise further awareness of the tool and also expand this intervention to other medications.
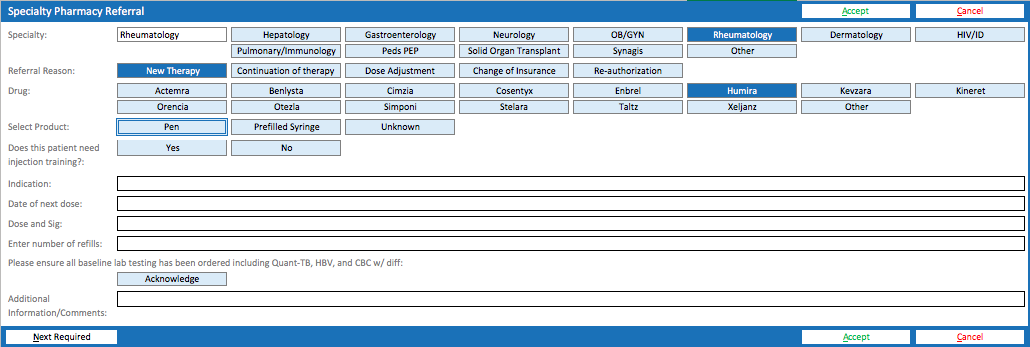 Figure 1a. Pre-Intervention Referral Shell. The previous order only allows providers to select a single medication without any alternatives in the event that the medication is denied.
Figure 1a. Pre-Intervention Referral Shell. The previous order only allows providers to select a single medication without any alternatives in the event that the medication is denied.
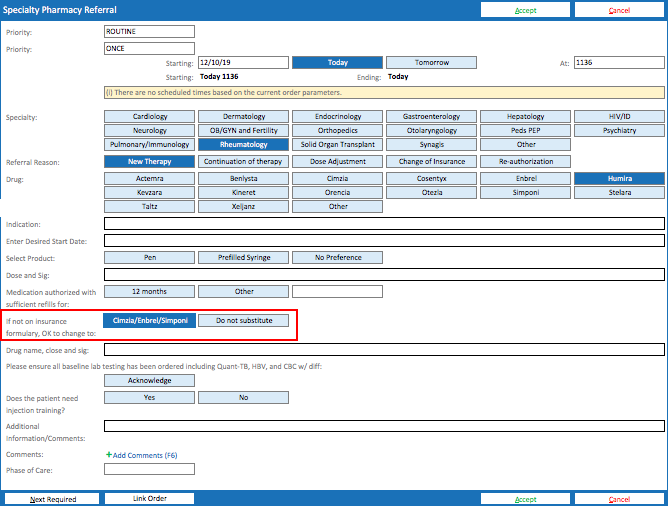 Figure 1b. Post-Intervention Referral Shell. The new order allows providers to select a replacement medication within the same class if the initial medication is not approved as shown by the red box.
Figure 1b. Post-Intervention Referral Shell. The new order allows providers to select a replacement medication within the same class if the initial medication is not approved as shown by the red box.
 Figure 2: Specialty Pharmacy (SP) Referral Process Map. This map was created by our multidisciplinary group to identify all steps in our SP referral process and identify areas of delay within the process. Using time-driven activity-based costing (TDABC), a tool used to estimate the cost of processes in different sectors such as health care, we measured the amount of time (in minutes), noted in yellow circles, needed to complete each step in the process. This allowed us to generate an estimate for the cost of each SP referral.
Figure 2: Specialty Pharmacy (SP) Referral Process Map. This map was created by our multidisciplinary group to identify all steps in our SP referral process and identify areas of delay within the process. Using time-driven activity-based costing (TDABC), a tool used to estimate the cost of processes in different sectors such as health care, we measured the amount of time (in minutes), noted in yellow circles, needed to complete each step in the process. This allowed us to generate an estimate for the cost of each SP referral.
To cite this abstract in AMA style:
Waytz J, Sultan D, Patel V. Reducing Delays for Biologic Medication Approval in Outpatient Rheumatology [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/reducing-delays-for-biologic-medication-approval-in-outpatient-rheumatology/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/reducing-delays-for-biologic-medication-approval-in-outpatient-rheumatology/
