Session Information
Session Type: Poster Session B
Session Time: 9:00AM-10:30AM
Background/Purpose: Despite the efficacy of modern biologic and small molecule medications, a significant proportion of RA patients have inadequate response to multiple therapies. These patients often switch or “cycle” medications, and medication switching has been adopted as a key criterion of “difficult to treat” RA. However, inefficacy is just one of many reasons that RA patients may switch biologic or targeted synthetic DMARD (combined here as “b/tsDMARDs”). The objective of this study was to categorize the reasons for b/tsDMARD switching in a large RA cohort and determine clinical characteristics associated with RA treatment nonresponders.
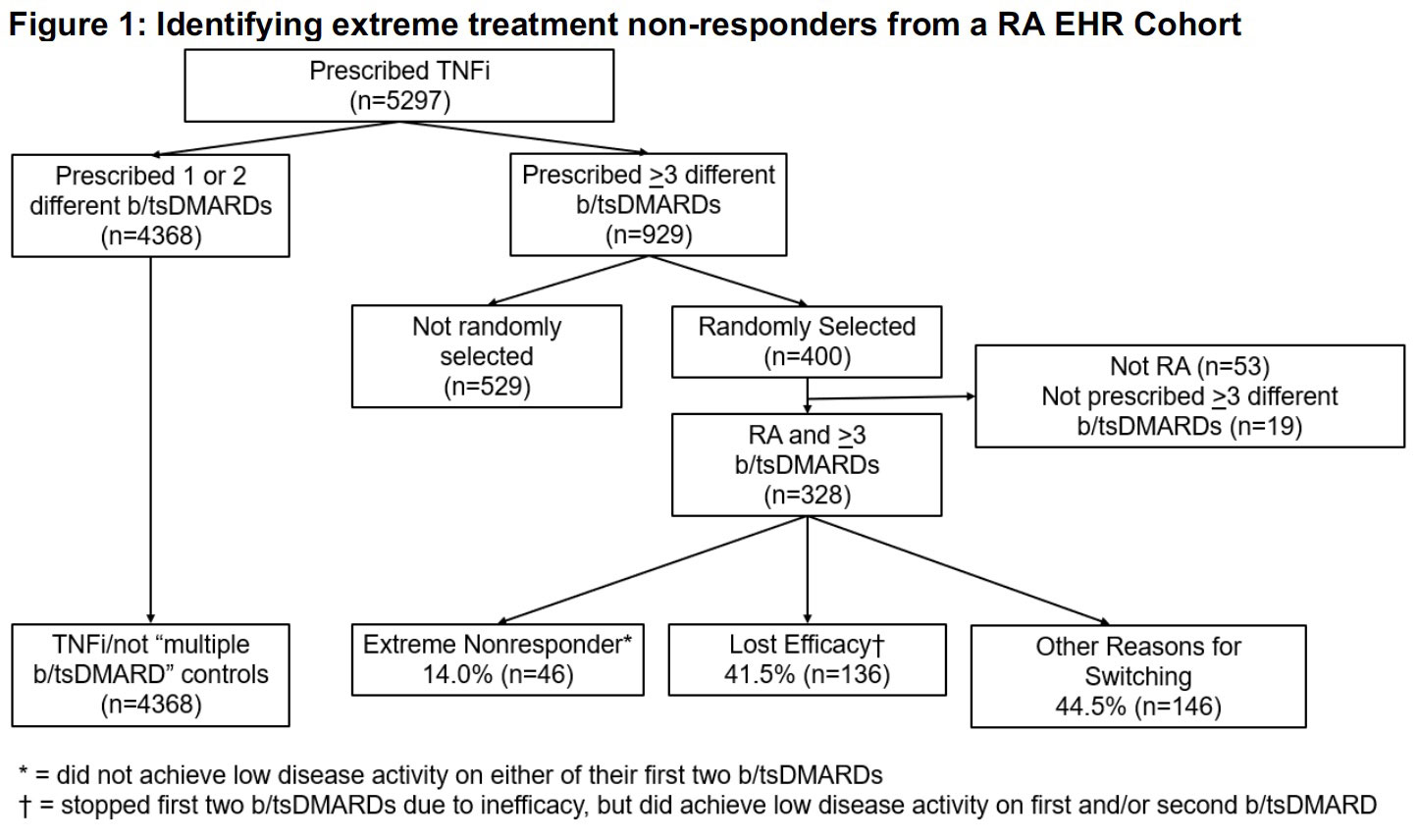
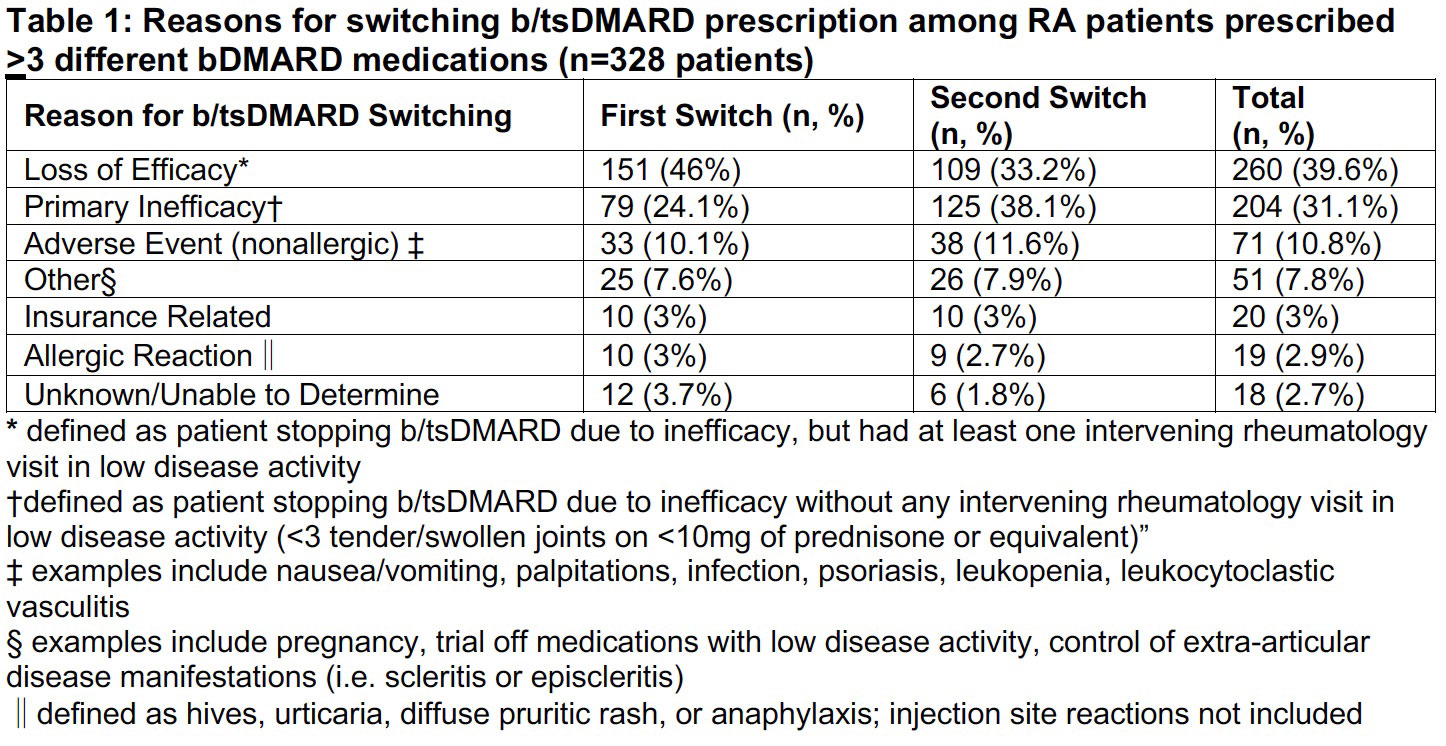
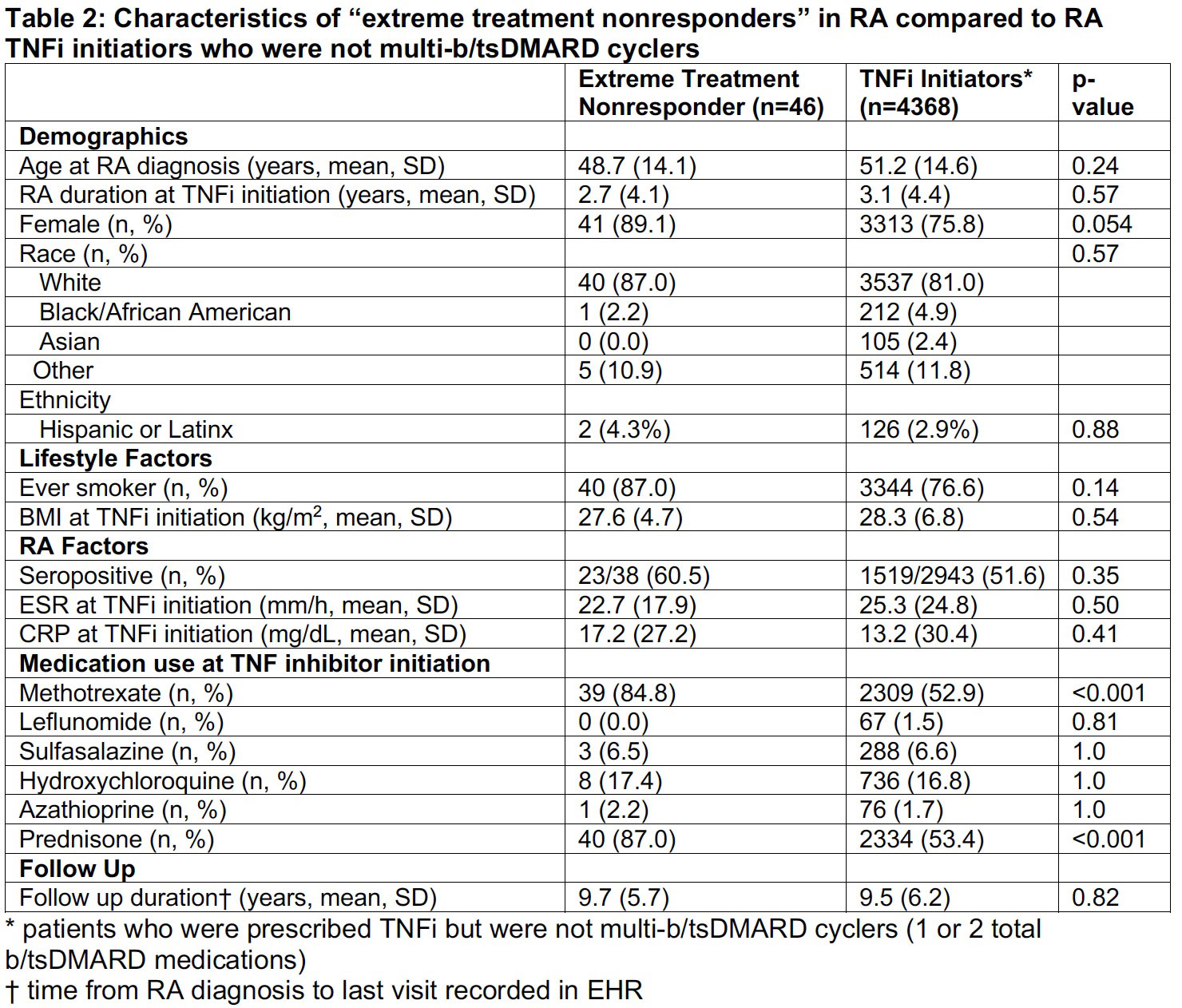
Methods: We studied RA patients with ≥1 TNF-α inhibitor (TNFi) prescription between 2001-2017 in a large multi-hospital electronic health record (EHR)-based RA cohort. To screen for RA treatment nonresponders, we selected patients who were prescribed ≥2 additional b/tsDMARD medications and randomly selected 400 patients for manual chart review to determine reasons for medication switching. After completing the review, we developed categories detailing reasons for medication switching. We further focused our analysis on the subgroup of “extreme treatment non-responders” who did not achieve low disease activity (e.g. < 3 tender or swollen joints on < 10mg of daily prednisone or equivalent glucocorticoid) on either of their first two b/tsDMARDs. We used descriptive statistics to compare demographic, lifestyle and RA clinical factors between “extreme treatment non-responders” and RA patients who initiated TNFi but were not treated with multiple b/tsDMARDs.
Results: In the RA cohort, 33% (n=5297) received TNFi. Of the TNFi initiators, 5.7% (n=929) were prescribed ≥2 additional b/tsDMARDs (multi b/tsDMARD) and served as the source of our random selection of patients for manual review (Figure 1). In this group, 82% (n=328) were confirmed to have RA treated with ≥3 b/tsDMARDs and 14.3% (n=47) were “extreme treatment non-responders.” We identified 8 categories for b/tsDMARD switching (Table 1). The most common reason for switching was loss of efficacy (39.6% of medication switches), followed by primary inefficacy and non-allergic adverse events (31.1% and 10.8% of medication switches, respectively). Extreme treatment non-responders were more likely than the TNFi-treated RA patients who were not multi-b/tsDMARD cyclers to have prescriptions for methotrexate (83.0% vs 52.9%, p< 0.001) or prednisone (85.1% vs 53.5%, p< 0.001) in the year preceding TNFi initiation. There was a trend towards an increased proportion of female patients (89.1% vs. 75.8%, p=0.054) and ever smokers in the extreme non-responder group (87.2% vs 76.7%, p=0.138) that did not reach statistical significance.
Conclusion: RA patients frequently switch b/tsDMARDs and the most common reasons for switching were loss of efficacy followed by primary inefficacy. Notably, nonallergic adverse events (e.g infections, leukopenia, psoriasis) comprised the third largest category. Clinical factors are insufficient for differentiating b/tsDMARD responders from nonresponders, highlighting the need for additional serologic and genetic biomarkers to inform treatment decisions.
To cite this abstract in AMA style:
McDermott G, Dahal K, Moon S, Seyok T, Weisenfeld D, Liao K. Reasons for Multiple Biologic DMARD Switching and Characteristics of “Extreme Treatment Nonresponders” in Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/reasons-for-multiple-biologic-dmard-switching-and-characteristics-of-extreme-treatment-nonresponders-in-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/reasons-for-multiple-biologic-dmard-switching-and-characteristics-of-extreme-treatment-nonresponders-in-rheumatoid-arthritis/