Session Information
Date: Tuesday, October 23, 2018
Title: Systemic Lupus Erythematosus – Clinical Poster III: Treatment
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose:
Systemic lupus erythematosus (SLE) has a 27.2% all-cause 30 day readmission rate, the 6th highest principle diagnosis among all medical conditions. The primary objective of the current study was to determine the 30-day all-cause readmission rate for adults with SLE at Wake Forest Baptist Medical Center (WFBMC). The secondary objective was to determine risk factors associated with 30-day readmission.
Methods:
Using the electronic medical record, we conducted a retrospective chart review of patients who met the following criteria: ICD 9 code for SLE, age >18, and had at least one hospital admission within a 2-year study period (8/1/2012-7/31/2014). Individual charts were manually reviewed to validate the diagnosis of SLE. Planned hospitalizations were excluded. The primary outcome was all cause-readmission within 30 days of initial hospital discharge. We recorded demographics, health care system-related variables and clinical data including comorbidity illness burden using the Charlson Comorbidy Index (CCI).
Results:
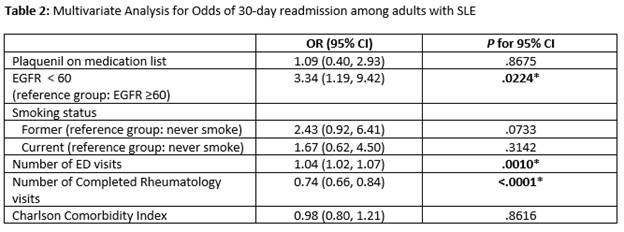
Over a 24 month period there were a total of 74 unique patients with SLE who had a total of 233 admissions. Of these 233 admissions, 82 (35.2%) were 30-day readmissions. The mean age of the cohort was 43.8 (SD 14.22), 85.1% female, 67.6% African Americans and 23.0 % on Medicaid/self-pay. Of these 74 patients, 27 (36.5%) had at least one 30-day readmission and contributed to 70% of total admissions. On bivariate analysis, serositis, higher CCI, estimated GFR <60, greater number of ER visits and less frequent rheumatology clinic visits were significant predictors of 30-day readmission. On multivariate analyses, significant predictors of 30-day readmission included estimated GFR < 60 (OR 3.34; p=.0224), presence of serositis as a prior criterion for lupus diagnosis (OR 11.87; p=.0071), and more frequent ER visits (OR 1.04; p=0.0010). More frequent rheumatology clinic visits (OR 0.74; p=<.0001) was associated with less readmission during the 2-year study period.
Conclusion:
We found a 35.2% 30-day readmission rate that was substantially higher than the previously cited 27.2% readmission rate. Serositis (as a criterion in SLE diagnosis), EGFR < 60, and more frequent ED visits were associated with increased rate of 30-day readmissions. On the other hand, higher number of completed rheumatology visits was associated with less frequent 30-day readmissions. Surprisingly, demographics, median household income, insurance payer status, and lupus disease activity including the use of immune-suppressant at index admission were not significant predictors of readmission.
To cite this abstract in AMA style:
Mullis S, Ang D. Rates and Predictors of Thirty-Day Readmission Among Patients Hospitalized for Systemic Lupus Erythematosus at a Single Tertiary Care Center [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/rates-and-predictors-of-thirty-day-readmission-among-patients-hospitalized-for-systemic-lupus-erythematosus-at-a-single-tertiary-care-center/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/rates-and-predictors-of-thirty-day-readmission-among-patients-hospitalized-for-systemic-lupus-erythematosus-at-a-single-tertiary-care-center/