Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Patients with systemic lupus erythematosus (SLE) have been shown to have increased burden of multimorbidity. Racial disparities in multimorbidity have also been shown repeatedly. We aimed to study variation in multimorbidity among SLE patients of different racial backgrounds.
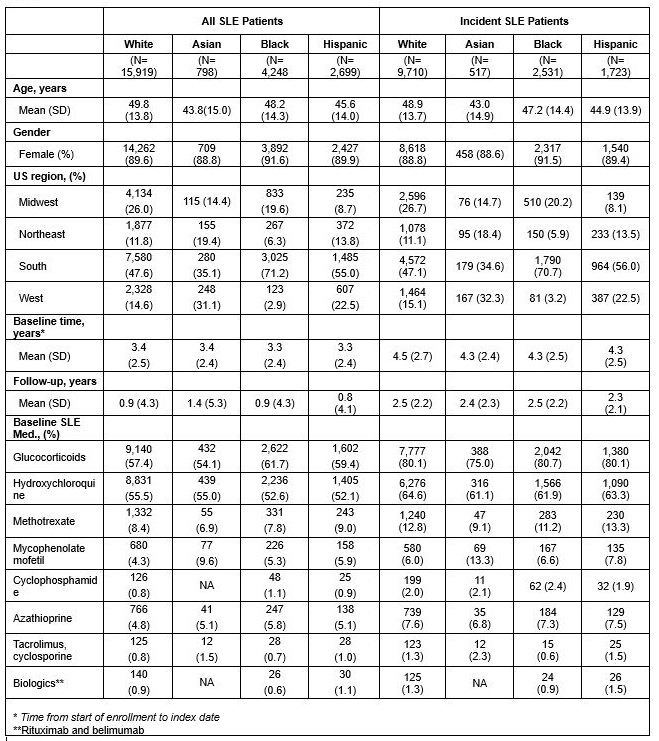
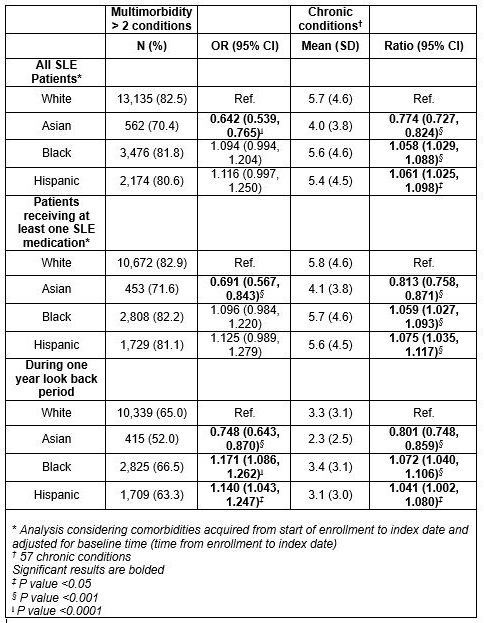
Methods: We identified patients with SLE included in the OptumLabs Data Warehouse, a real-world data asset with de-identified administrative claims and clinical information for commercial and Medicare Advantage enrollees January 2006 through September 2015. Cases were defined as patients with ≥3 SLE ICD-9 codes between January 2006 and September 2015 with incident cases identified by absence of SLE codes for at least one year prior to the index date. Race was classified as non-Hispanic Asian (Asian), non-Hispanic Black (Black), non-Hispanic White (White), and Hispanic based on derived rule sets. Multimorbidity (2 or more comorbidities excluding SLE) was defined using 57 pre-defined chronic comorbidities. Two or more ICD-9 codes were used to define a comorbidity. The Non-Hispanic White SLE cohort- the largest group, was used as the reference. Logistic regression models were used to estimate odds ratios (OR) with 95% confidence intervals (CI) adjusted for age, sex, and disease duration. Comorbidity burden (number of comorbidities) between the non-White SLE groups and Non-Hispanic White SLE group (reference) were compared using negative binomial regression and adjusting for age, gender, and baseline time. Chronic condition accrual was determined using generalized estimating equations and adjusting for age and sex with multiple sensitivity analyses.
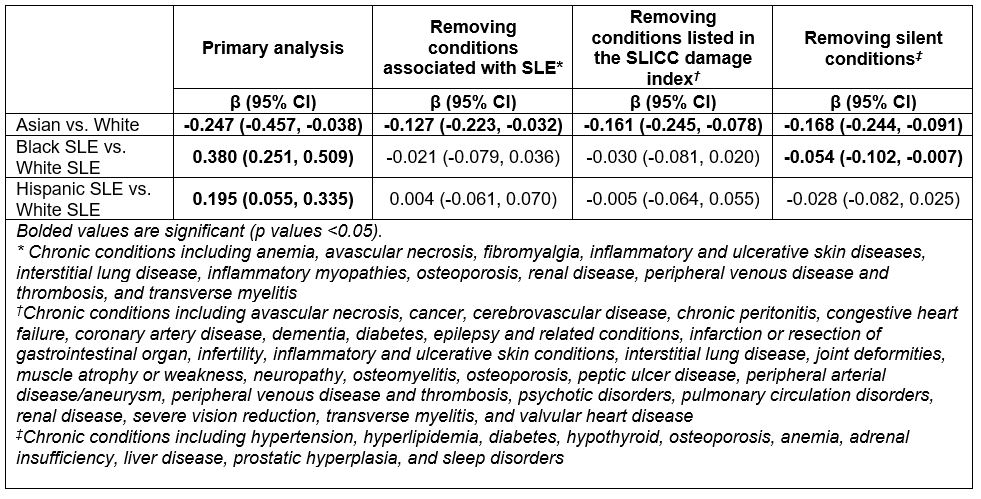
Results: 23,664 SLE patients were included in this study with 90% female, 3.4% Asian, 18.0% Black, 11.4% Hispanic, and 67.3% White. 14,481 incident cases were identified with similar sex and racial distribution. Mean follow-up was 0.9 ± 4.3 years in the total cohort and 2.5 ± 2.2 years in the incident cohort. Odds of multimorbidity was significantly lower in Asian patients (OR 0.642 95% CI 0.539 – 0.765) compared to White patients and not significantly different in Black or Hispanic patients. Comorbidity burden was lower in Asian patients (Ratio 0.774 95% CI 0.727-0.824 and higher in Black (Ratio 1.058 95% CI 1.029-1.088) and Hispanic patients (Ratio 1.061 95% CI 1.025-1.098) compared to White patients with SLE. Rate of comorbidity accrual was significantly lower in Asian patients with SLE even after removal of conditions associated with SLE, those associated with SLE damage, and silent conditions while the higher accrual rate in Black and Hispanic patients did not persist with removal of these comorbidities. Multiple sensitivity analyses were done to validate results.
Conclusion: Among patients with SLE with commercial insurance or Medicare Advantage plans, racial disparities in multimorbidity, comorbidity burden, and comorbidity accrual were present, with Asian patients demonstrating lower burden of chronic diseases and Black and Hispanic patients being disproportionately affected.
To cite this abstract in AMA style:
Williamson K, Heien H, Stevens M, Crowson C, McCoy R, Duarte-Garcia A. Racial/Ethnic Variation in Multimorbidity Risk and Accrual and Comorbid Conditions Among Patients with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/racial-ethnic-variation-in-multimorbidity-risk-and-accrual-and-comorbid-conditions-among-patients-with-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/racial-ethnic-variation-in-multimorbidity-risk-and-accrual-and-comorbid-conditions-among-patients-with-systemic-lupus-erythematosus/