Session Information
Date: Sunday, November 12, 2023
Title: (0176–0195) Healthcare Disparities in Rheumatology Poster I: Lupus
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
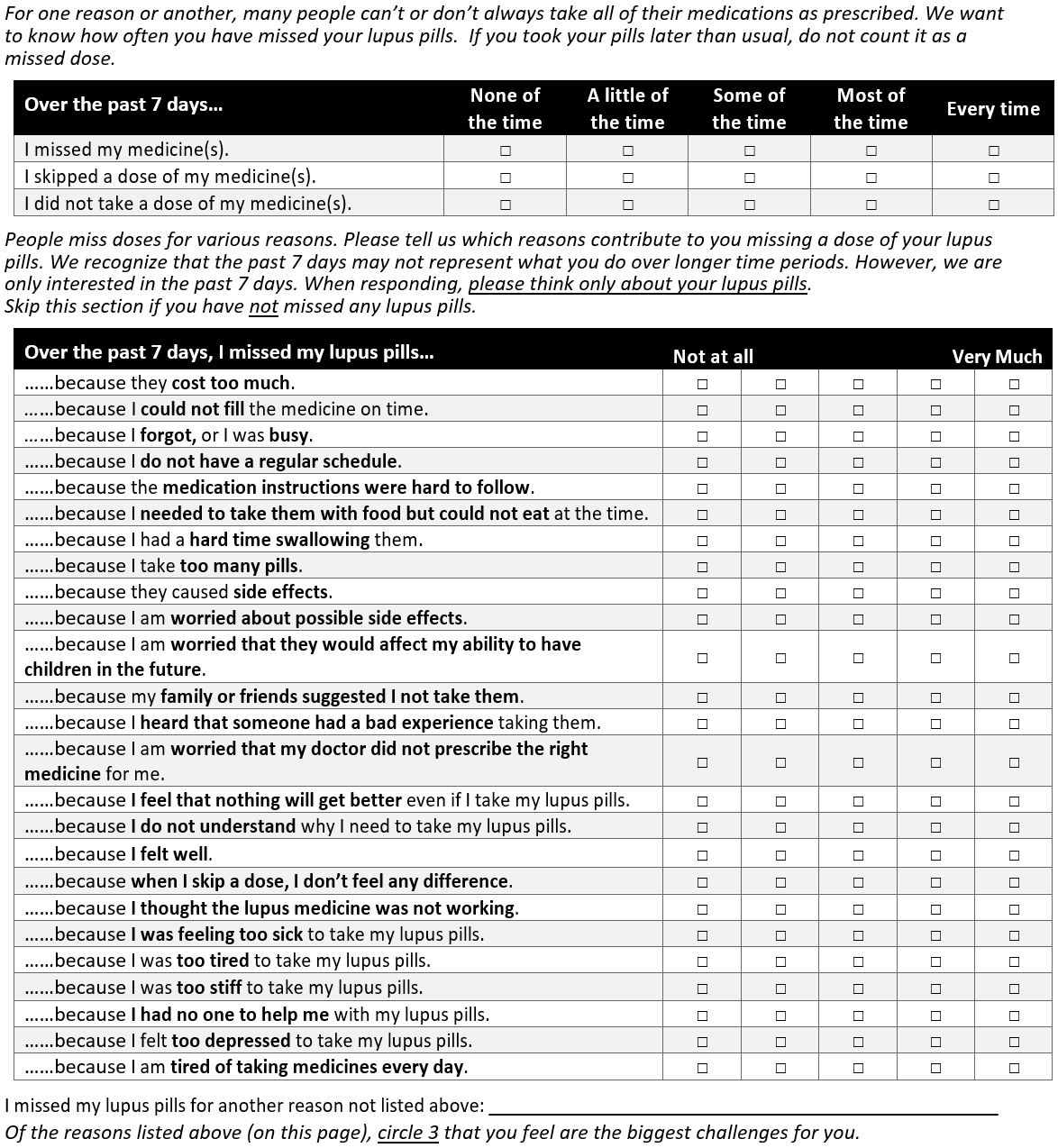
Background/Purpose: Medication nonadherence is common in SLE and disproportionately affects Black patients. Nonadherence leads to increased hospitalizations, morbidity, and mortality and is a modifiable factor that can reduce racial disparities in SLE outcomes. To better recognize nonadherence and address adherence barriers, we previously adapted and validated a self-reported measure of extent of nonadherence and reasons for nonadherence called Domains of Subjective Extent of Nonadherence (DOSE- nonadherence-SLE) (Figure 1). In this study, we examined frequencies of reasons for nonadherence to explore possible item reduction and reasons that disproportionately affect Black patients.
Methods: Patients from an academic clinic who met ACR or SLICC criteria for SLE and were prescribed ≥1 SLE medication completed demographic information and the DOSE-Nonadherence-SLE survey, which measures the extent of and reasons for nonadherence over the past 7 days. We limited the analysis to include only patients who self-identified as Black or White race due to small numbers of patients who self-identified as belonging to other races. We compared racial differences in reasons for nonadherence using Chi squared or Fisher’s exact tests. We used step-wise multivariable logistic regression to examine factors independently associated with reasons that differentially affected Black patients.
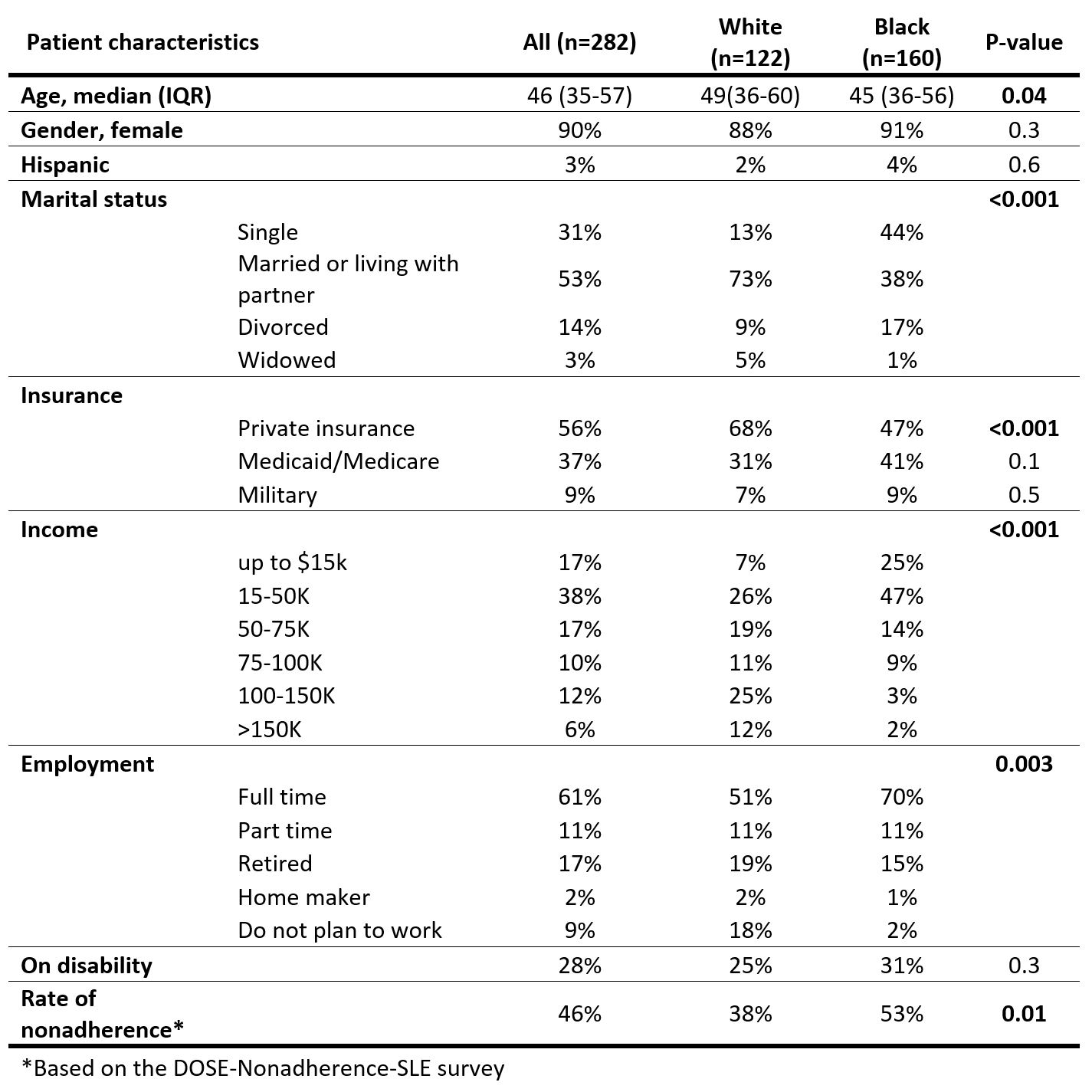
Results: A total of 282 surveys were completed (median age 47, 90% female, 57% Black, 94% HCQ, 48% MMF, 13% AZA, 10% MTX). Black compared to White patients were more likely to be single, working full time, have annual household income < $50,000, and less like to have private insurance (Table 1).
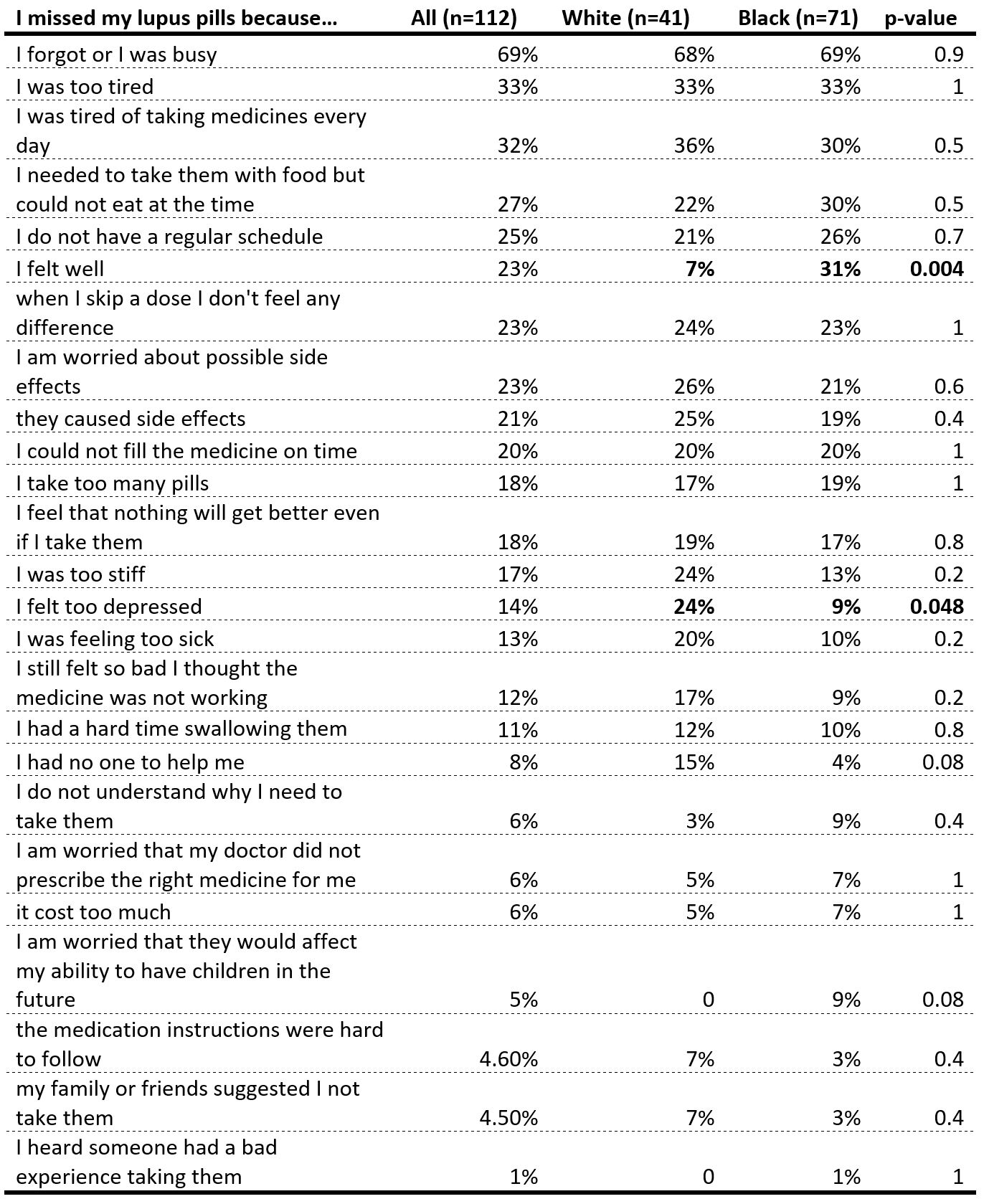
Rates for nonadherence were 53% among Black patients compared to 38% among White patients (p=0.01). The most common reasons for nonadherence were “I forgot or I was busy” (69%), “I was too tired” (33%), and “I am tired of taking medicines every day” (32%). The least common reasons were missing doses due to “the medication instructions were hard to follow” (4.6%), “my family or friend suggested I not take them” (4.5%), and “I heard that someone had a bad experience taking them” (1%).
Most reasons for nonadherence were reported at similar rates by Black and White patients (Table 2). However, Black compared to White patients were more likely to report missing doses due to “I felt well” (31% vs 7%, p=0.004) and “I am worried that the medicine would affect my ability to have children in the future” (9% vs. 0, p=0.08), whereas White patients were more likely to report missing doses due to “I felt too depressed” (24% vs. 9%, p=0.048) and “I had no one to help me” (15% vs 4%, p= 0.08). After adjusting for other demographic factors, nonadherent due to feeling well was dependently associated with Black race (OR 15, p=0.001).
Conclusion: While busyness and forgetting, physical fatigue, and pill fatigue commonly affect all patients, Black patients were much more likely to report missing doses due to feeling well, and there is a trend that Black patients were more concerned about medication effects on fertility. These represent unique opportunities to improve adherence for Black patients. Our results also suggest that some items can be eliminated to reduce response burden due to their low frequencies.
To cite this abstract in AMA style:
Sun K, Robinson L, Eudy A, Rogers J, Sadun R, Criscione-Schreiber L, Doss J, Clowse M. Racial Disparities in Self-reported Extent and Reasons for Nonadherence in SLE [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/racial-disparities-in-self-reported-extent-and-reasons-for-nonadherence-in-sle/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/racial-disparities-in-self-reported-extent-and-reasons-for-nonadherence-in-sle/