Session Information
Date: Sunday, November 7, 2021
Title: Plenary II (0956–0961)
Session Type: Plenary Session
Session Time: 10:30AM-10:45AM
Background/Purpose: Racial and ethnic minorities are disproportionately affected by pediatric-onset SLE and have worse outcomes compared to their white counterparts. With ongoing advances in pediatric SLE care, it is not known how these gaps are changing. We determined whether changes in renal outcomes over time of hospitalized children with SLE varied by race/ethnicity, and whether these trends differed by hospital minority composition.
Methods: We identified patients ≤21 years old with an ICD-9/10 hospital discharge diagnosis of SLE in the Pediatric Health Information System® inpatient database from 2006-2019. Adverse renal outcomes were defined by assignment of an end-stage renal disease (ESRD) diagnosis code, dialysis procedure code, or renal transplant, analyzed separately and as a composite outcome. We used logistic regression models with fixed effects for time (calendar period), demographic and disease characteristics, and hospital-level random effects to estimate odds of a) an adverse renal outcome at any single hospital encounter or b) incident hospitalization for an adverse renal outcome, after which subsequent encounters were censored. We tested interactions between race and time to assess if change over time differed by race/ethnicity. Hospitals were further dichotomized by whether ≥50% of SLE patients were Black or ≥50% were Hispanic (Creanga et al. 2014) to test multiplicative interactions between hospital minority composition, race and time.
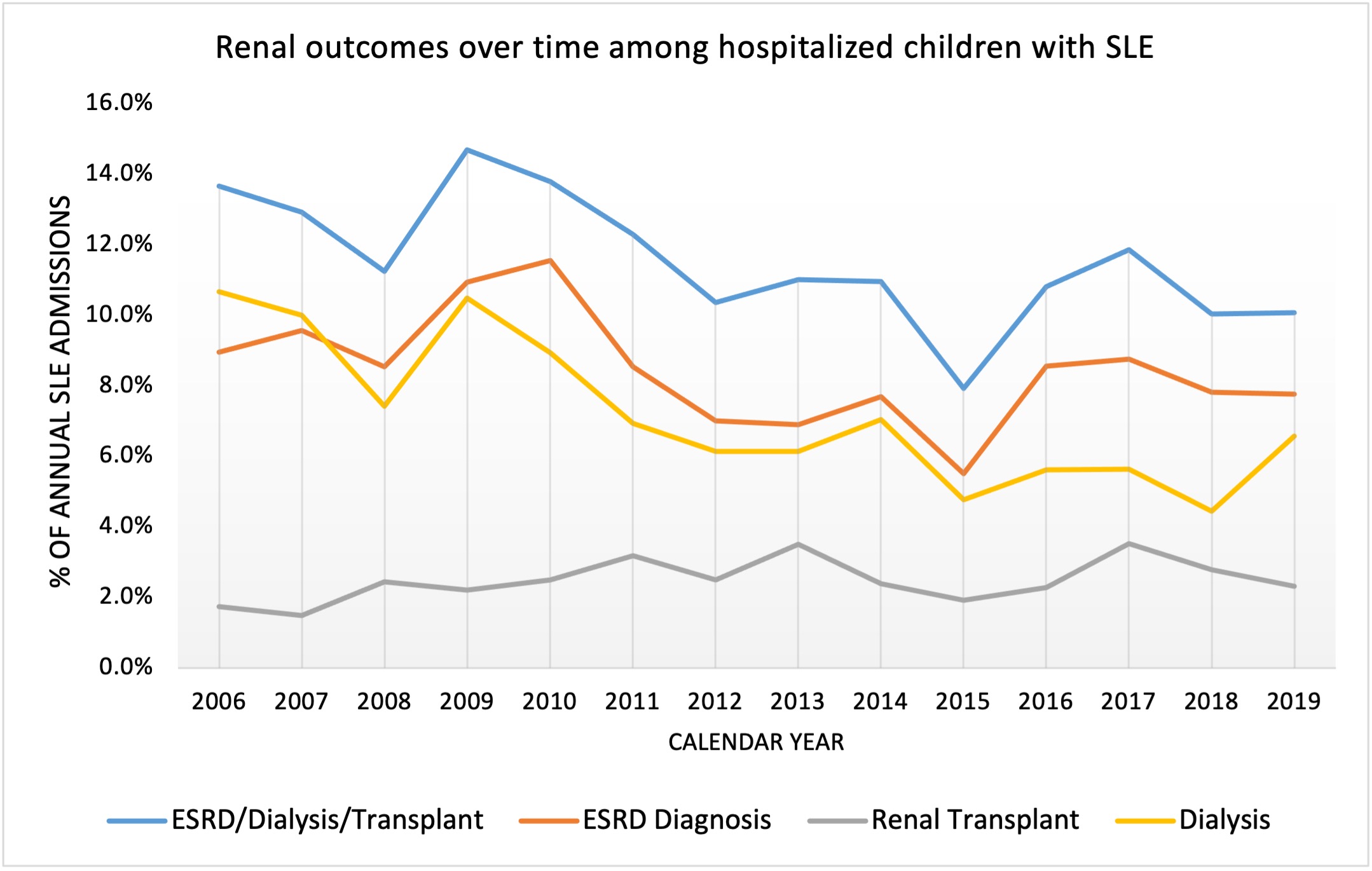
Results: There were 7,434 unique SLE patients with a total of 20,893 admissions at 50 hospitals. Racial/ethnic composition and patient characteristics are shown in Table 1. The proportion of SLE admissions with any adverse renal outcome, ESRD, or dialysis decreased over time from 2006 to 2019 (Fig. 1, p< 0.01 for trends). However, Black children remained significantly more likely to have an adverse renal outcome at any hospital encounter (adjusted OR 2.5, 95% CI [1.8-3.5]) over time compared to non-Hispanic whites. Black and Asian children were also more likely to have an incident hospitalization for an adverse renal outcome (OR 1.4 [1.1-1.8] and OR 1.5 [1.0-2.4], respectively). There were no significant changes in the magnitude of disparity over time. However, there were significant differences in both the magnitudes of disparities and changes in disparity levels over time between hospitals in which Black or Hispanic minorities comprised ≥50% of SLE patients vs. < 50% (p-values for interactions < 0.01). At hospitals with ≥50% Hispanic SLE patients, renal outcomes failed to improve at the same rate among Black and Hispanic white patients compared to non-Hispanic whites (Fig. 2A/B). At hospitals with ≥50% Black SLE patients, rates of renal outcomes improved less over time among black vs. non-Hispanic white children and worsened among Hispanic white children (Fig. 2C/D).
Conclusion: On average, adverse renal outcomes among hospitalized children with SLE decreased over a 13 year period, but racial disparities persisted without significant narrowing of the existing gap. There is a specific need to address greater or widening disparities that are systematically concentrated in local contexts despite population level improvements.
To cite this abstract in AMA style:
Chang J, Sears C, Torres V, Son M. Racial Disparities in Renal Outcomes over Time Among Hospitalized Children with SLE and Effects of Hospital Minority Composition [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/racial-disparities-in-renal-outcomes-over-time-among-hospitalized-children-with-sle-and-effects-of-hospital-minority-composition/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/racial-disparities-in-renal-outcomes-over-time-among-hospitalized-children-with-sle-and-effects-of-hospital-minority-composition/