Session Information
Date: Monday, November 13, 2023
Title: (1442–1487) SLE – Diagnosis, Manifestations, & Outcomes Poster II
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Lupus nephritis (LN) is a significant predictor of morbidity and mortality in Systemic Lupus Erythematosus (SLE). Racial disparities are known to exist in SLE in terms of the prevalence of LN, healthcare access, and outcomes. We aimed to study racial disparities in LN and predictors of in-hospital death.
Methods: Data was obtained from the National Inpatient Sample (NIS) between 2016-2019 using ICD-10 codes. All adult hospitalizations with a primary or secondary diagnosis of LN were included and divided into African American (AA) and Hispanic race vs others. Demographics, socio-economic variables, several complications, health care burden, and mortality were compared between the two groups. Univariate and multivariate logistic regression analyses were conducted for predictors of in-hospital death in LN. Variables with a P value ≤0.2 in the univariate analysis were included in the multivariate model and a P value of ≤0.05 was considered to be significant in the final model.
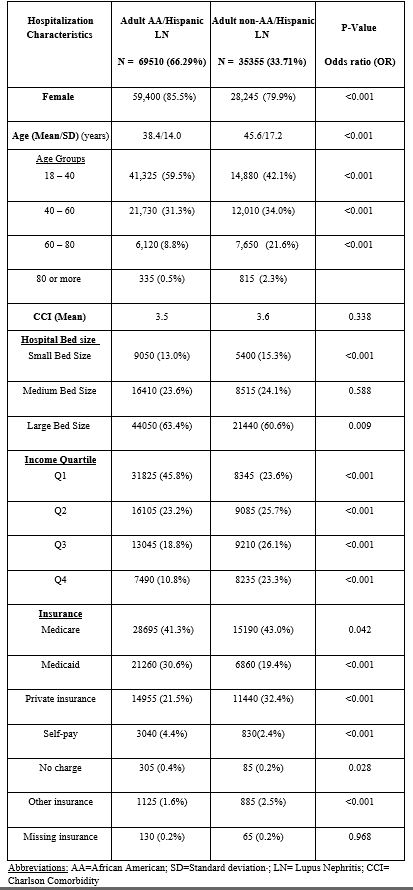
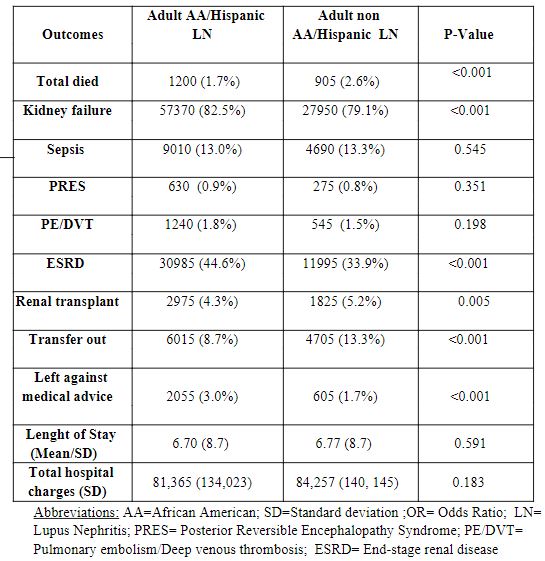
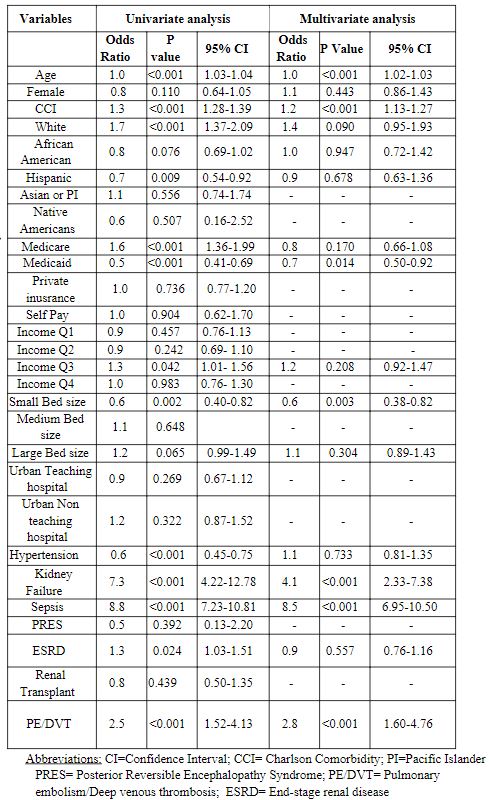
Results: We identified 104, 865 adult LN hospitalizations, of which 66.3% were African Americans or Hispanics (table 1). This group had more females (85.5% vs 79.9%, p< 0.001), were younger (38.4 vs 45.6 years, p< 0.001),were more likely to be from the low-income group (45.8% vs 23.6%, p< 0.001) and more often had Medicaid (30.6% vs 19.4% p< 0.001) in comparison to other races. In-patient mortality was low overall with lower odds of death in the AA-Hispanic group (1.7% vs 2.6%, OR 0.67, p< 0.001) (table 2).AA/ Hispanic LN patients had higher odds of renal failure (82.5% vs 79.1%, OR 1.25, p< 0.001) and end-stage renal disease (ESRD) (44.6% vs 33.9%,OR 1.6, p< 0.001) but were less likely to receive a renal transplant (4.3% vs 5.2%, OR 0.8, p=0.005). They were more likely to leave against medical advice (3.0% vs 1.7%, OR 1.8, p< 0.001,)and less likely to be transferred to a skilled nursing facility (8.7% vs 13.3%,OR 0.6, p< 0.001). Multivariable analysis for predictors of in-hospital death in LN showed following significant variables: Age (OR 1.0, p< 0.001), CCI (OR 1.2, p< 0.001), Medicaid (OR 0.7, p=0.014), small bed size (OR 0.6, p=0.003), sepsis (OR8.54, p< 0.001), PE/DVT (OR 2.8, p< 0.001), and kidney failure (OR4.1, p< 0.001) (table 3).
Conclusion: In the national inpatient sample, almost two-thirds of LN patients were AA or Hispanic. This group had a higher proportion of females, was younger, belonged more often to the lower income quartile, and was more likely to have Medicaid insurance. They had higher odds of renal failure and ESRD in comparison to other races and were less likely to receive renal transplants. The in-hospital mortality was lower in the AA/Hispanic-LN group, but race was not found to be an independent predictor of death in LN. Sepsis, kidney failure, PE/DVT, Charlson comorbidity index, and age were associated with higher odds of in-hospital death in LN.
To cite this abstract in AMA style:
Sami F, Sami S, Manadan A, Arora S. Racial Disparities in Lupus Nephritis: A Nationwide Analysis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/racial-disparities-in-lupus-nephritis-a-nationwide-analysis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/racial-disparities-in-lupus-nephritis-a-nationwide-analysis/