Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Medication non-adherence is common among SLE patients and is disproportionately more frequent in underrepresented racial minorities. We examined adherence gaps between minority and Caucasian SLE patients and explored factors associated with non-adherence that may present avenues for intervention.
Methods: Cross-sectional data were obtained via survey and chart review from consecutive SLE patients with ≥1 prescribed lupus medication. The Medication Adherence Self-Report Inventory (MASRI) was used to estimate adherence in the preceding month from 0-100%. High Self-reported Adherence was defined as MASRI ≥90%. Pharmacy refill data in the preceding 3 months were obtained by phone calls. High Refills was defined as a medication possession ratio of ≥80% for all prescribed SLE medications. High Composite Adherence was defined as having both High Self-reported Adherence and High Refills. Patient-provider interaction was measured using the Interpersonal Processes of Care survey, which has 7 domains on a 5-point Likert scale. Additional covariates included: self-efficacy, patient-reported health status, rheumatic medication regimen complexity, SLEDAI, Systemic Lupus Activity Questionnaire (SLAQ), and SLICC damage scores. Adherence measures were compared by race, and adherence groups were compared.
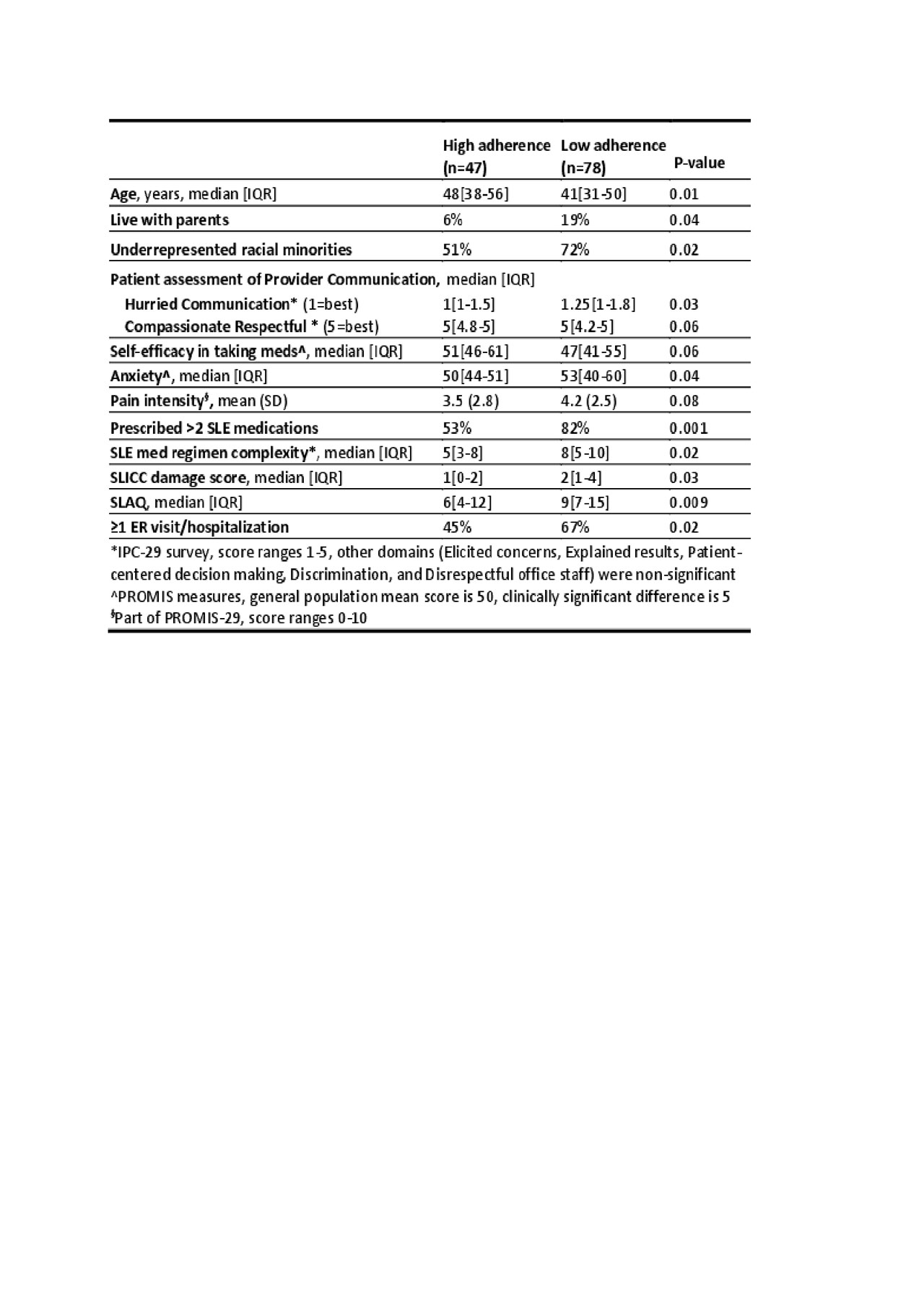
Results: 125 enrolled (36% Caucasians, 61% African American, 3% other). Median age was 43 (range 22-72), 95% were female, 51% had ≥ college education, and 49% had private insurance. 83 (66%) had High Self-reported Adherence, 59 (47%) had High Refills, and only 48 (38%) had High Composite Adherence. Minorities compared to Caucasians had lower rates of Self-Reported Adherence (58% vs 82%, p=0.005), Refills (40% vs. 60%, p=0.03), and Composite Adherence (30% vs. 61%, p=0.02). Among 75 taking disease modifying agents including MTX, LEF, AZA, and MMF, High Refill rate was 37% vs. 64% (p=0.03) for minorities compared to Caucasians. The racial gap in High Refill rate is largest for those on MMF (39% vs. 88%, p=0.01). Compared to the High Composite Adherence group, those with Low Composite Adherence were younger, more likely to live with parents, rated more Hurried communication with providers, had more anxiety, took a more complex SLE regimen, had higher SLICC Damage score, SLAQ, and more ER visits/hospitalizations. They also had a trend for less compassionate and respectful interaction with providers and lower self-efficacy in managing medications and treatments (table 1).
Conclusion: Significant racial disparities exist in SLE medication adherence, and the gap is most substantial for patients taking MMF, a crucial treatment for moderate to severe SLE. This gap likely contributes to known racial disparities in SLE outcomes. Improving communication, self-efficacy, mental health, and reducing medication burden may be avenues for intervention for a subset of non-adherent patients. Qualitative studies are needed to better understand barriers to adherence and to develop interventions that address this pressing racial disparity.
To cite this abstract in AMA style:
Sun K, Eudy A, Rogers J, Criscione-Schreiber L, Doss J, Sadun R, Clowse M. Racial Disparities in Lupus Medication Adherence [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/racial-disparities-in-lupus-medication-adherence/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/racial-disparities-in-lupus-medication-adherence/