Session Information
Session Type: Poster Session D
Session Time: 8:30AM-10:30AM
Background/Purpose: Racial heterogeneity of the US population makes it imperative to study the racial differences in clinical characteristics, medication use and co-morbidities of PsA patients to reduce the disparities in health care. We hypothesize that African-Americans (AA) with PsA have higher burden of co-morbidities then Caucasians in the US. We aimed to examine the racial differences in clinical characteristics, medication usage and co-morbidities in PsA patients.
Methods: We conducted a retrospective study using the IBM Explorys platform, a clinical research informatics tool that utilizes a health data gateway (HDG) server behind the firewall of 26 major integrated healthcare systems in the US from 1999, comprising of over 60 million patients in the participating healthcare organizations. The Explorys collects aggregated, standardized and normalized clinical data from different electronic health records, automatically updated in near real time (at least every 24 h), presented in a HIPAA and HITECH-compliant de-identified way from each participating healthcare organization and are passed into the Explorys data grid. Diagnosis, findings, and procedures are mapped into the systematized nomenclature of medicine (SONOMED-CT) hierarchy. Search criteria for PsA included the ICD diagnosis code of PsA and at least two visits with a rheumatologist, between 1999-2019. Cohorts were further stratified by adding the following variables to the search tool: race, gender, elevated ESR or CRP, smoker, peripheral arthritis, enthesopathy, dactylitis, uveitis, psoriasis, inflammatory bowel disease,TNF inhibitor or DMARD use) and co-morbidity (hypertension, diabetes, osteoporosis, fibromyalgia, heart disease and depression). Data sets were recorded as proportions and compared using chi-squared test (p< 0.05).
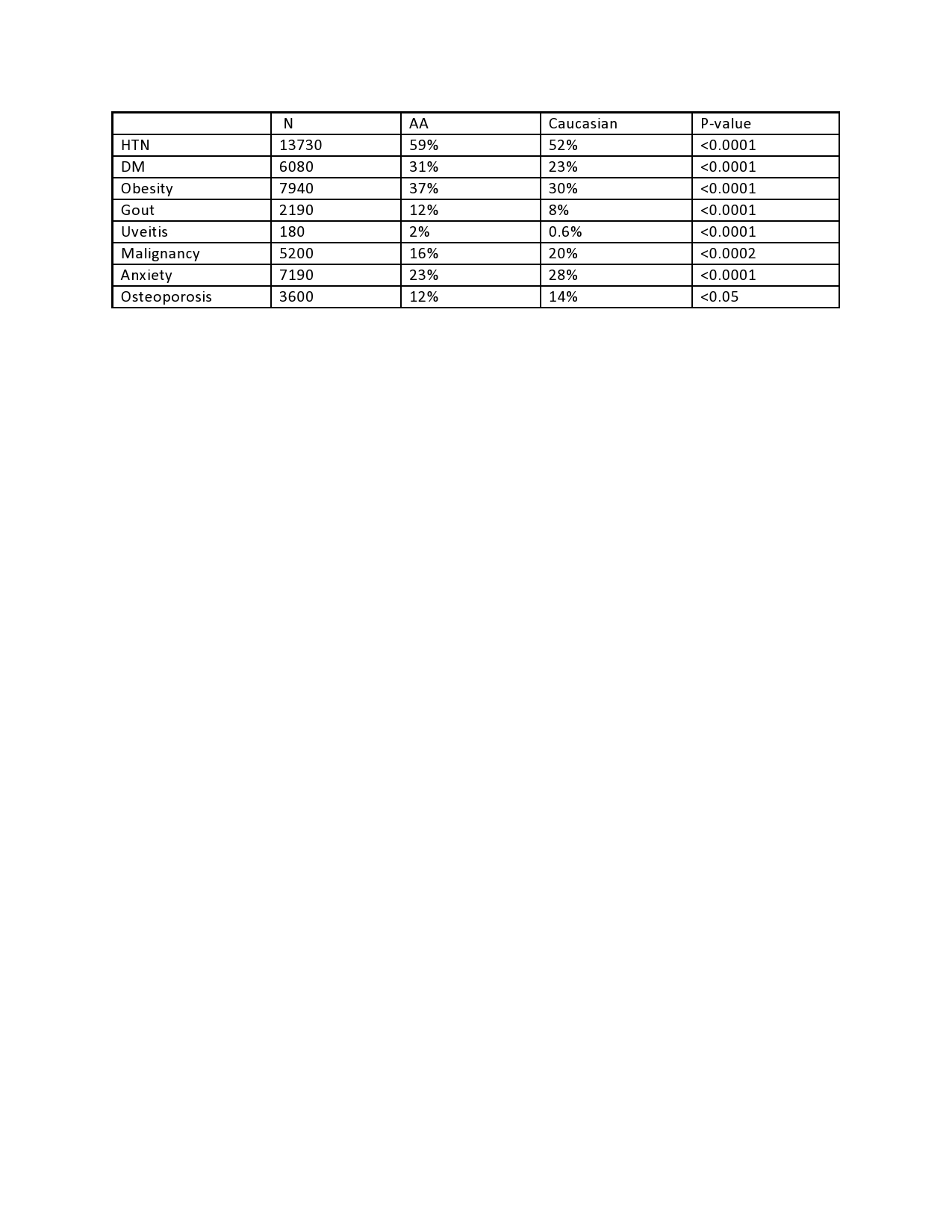
Results: A total of 26010 patients with PsA were identified. 95% of these patients were Caucasians whereas 5% were AA and 63% were females. 17% of PsA patients were smokers (n=4350) of which 4150 were Caucasians and 200 were AA, (p< 0.05). Comparisons of clinical features of PsA between racial groups can be found in Table 1. Treatment differences were also noted amongst racial groups. NSAIDs were used in 80% of Caucasians and 78% of AAs (p< 0.0097). TNFs were used in 51% of Caucasians and 41% of AAs (p< 0.0001). DMARDs were used in 72% of Caucasians and 98% of AAs (p< 0.0001). Significant difference in comorbidities between the 2 groups are shown in Table 2. Prevalence of other comorbidities including hyperlipidemia, coronary artery disease, depression and fibromyalgia were not significantly different among Caucasians and AA with PsA.
Conclusion: Our findings from a large US real world database revealed hypertension, diabetes, obesity, and gout were more prevalent in AA with PsA as compared to Caucasians. However, malignancy, osteoporosis and anxiety were more prevalent in Caucasians. The co-morbidities were significantly higher in AA patients with PsA and this warrants increased risk stratification. There was increased biologic use in Caucasians with PsA compared to AA who had a much higher use of DMARDs.
To cite this abstract in AMA style:
Jaleel S, Ross Y, Magrey M. Racial Disparities in Comorbidities of Patients with Psoriatic Arthritis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/racial-disparities-in-comorbidities-of-patients-with-psoriatic-arthritis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/racial-disparities-in-comorbidities-of-patients-with-psoriatic-arthritis/