Session Information
Date: Monday, November 8, 2021
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster III: Outcomes (1257–1303)
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: Black patients with systemic lupus erythematosus (SLE) face higher rates of morbidity and mortality compared to White patients. Long-term glucocorticoid use has been associated with worse health outcomes among patients with SLE. We sought to quantify chronic glucocorticoid use among Black and White patients with SLE within a prospective registry.
Methods: Using a registry at a large academic institution, we compared chronic glucocorticoid use among participants with SLE that self-identify as Black or White race. SLE was defined by either Systemic Lupus International Collaborating Clinics or American College of Rheumatology criteria. At the time of registry enrollment, demographic and disease specific variables, including age, sex, Systemic Lupus Erythematosus Disease Activity Index 2000 (SLEDAI-2k), hospitalization in the year before registry enrollment, disability status, and current SLE-related medications were captured. Chronic glucocorticoid utilization was defined as both documentation of current glucocorticoid use by participant self-report and physician documentation of steroid use as part of SLE treatment at the time of registry enrollment. Multivariable logistic regression of race and chronic glucocorticoid use was performed, adjusting for covariates exhibiting a bivariate association with chronic glucocorticoid use at significance level p< 0.10.
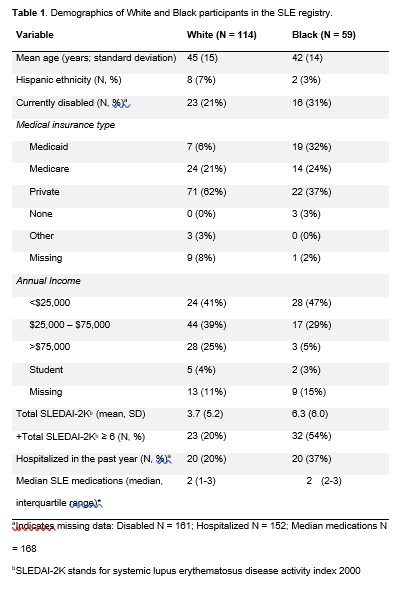
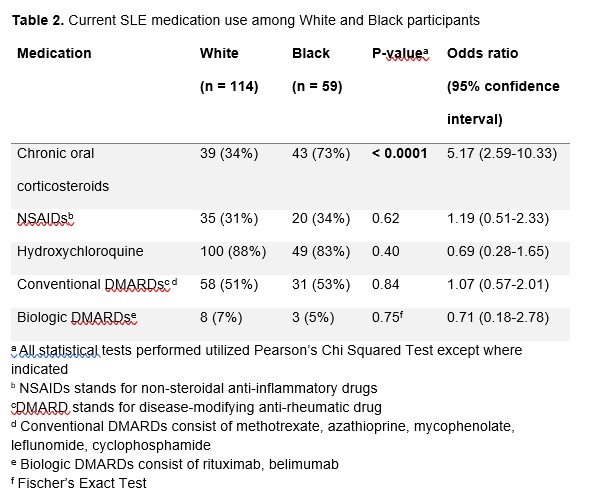
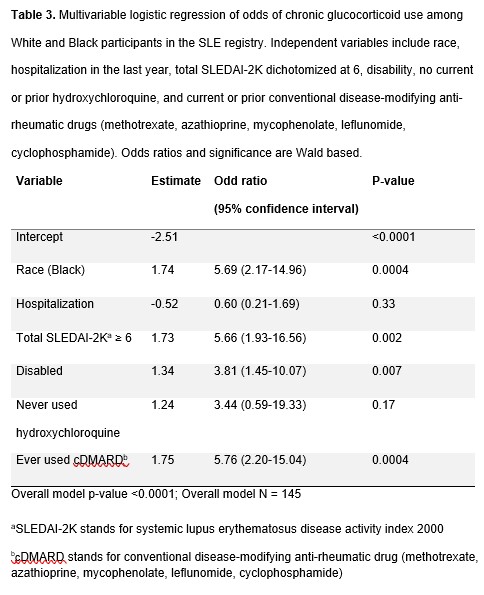
Results: 114 White participants (mean age 45; standard deviation (SD) 15) and 59 Black participants (mean age 42; SD 14) were analyzed. White participants had mean SLEDAI-2K score of 3.7 (SD 5.2). Black participants had mean SLEDAI-2K scores of 6.3 (SD 6.0). Among Black participants, 43 (72%) utilized glucocorticoids compared to White participants 39 (34%) (unadjusted odds ratio (OR) 5.17; 95% confidence interval (CI) 2.59-10.33). We did not observe differences between unadjusted hydroxychloroquine (OR 0.69; 95% CI 0.28-1.65) or conventional disease-modifying anti-rheumatic drug (cDMARD) (OR 1.07; 95% CI 0.57-2.01) utilization among Black and White participants. SLEDAI-2K, disability, recent hospitalization, and past or present hydroxychloroquine or cDMARD use were included in a logistic regression model. Adjusting for covariates, Black participants were more likely to be on glucocorticoids (adjusted OR 5.69; 95% CI 2.17-14.96); p=0.0004).
Conclusion: Adjusting for disease activity and other medications, Black patients had greater exposure to chronic glucocorticoids than White patients in a prospective SLE registry while cDMARD use remained the same. These patients may face increased glucocorticoid-related morbidity, which could contribute significantly to long-term health outcomes and utilization of health care resources. Future research in larger, more diverse registries should be conducted to further characterize patterns of glucocorticoid use.
To cite this abstract in AMA style:
Sullivan J, Littlejohn E. Racial Differences in Chronic Glucocorticoid Use in Patients with SLE: A Cross Sectional Study [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/racial-differences-in-chronic-glucocorticoid-use-in-patients-with-sle-a-cross-sectional-study/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/racial-differences-in-chronic-glucocorticoid-use-in-patients-with-sle-a-cross-sectional-study/