Session Information
Date: Saturday, November 6, 2021
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster I: Diagnosis (0323–0356)
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: Racial and ethnic minorities experience a disproportionate burden of systemic lupus erythematosus (SLE) as well as earlier development of lupus manifestations as compared to White individuals. Data on onset of lupus symptoms across multiple organ domains and in Asian patients in the US is lacking. We analyzed racial/ethnic differences in time to onset of renal, neuropsychiatric, hematologic, cardiovascular, and multiorgan disease following SLE diagnosis in a multi-ethnic cohort of patients.
Methods: The California Lupus Epidemiology Study (CLUES) is a longitudinal cohort of 431 individuals with SLE, of whom 332 participated in a baseline in-person study visit. Data on major end-organ manifestations including dates of onset were collected and confirmed by study rheumatologists. Manifestations of end-organ disease were categorized by organ system: renal (lupus nephritis), neuropsychiatric (seizure, stroke, mononeuritis multiplex, peripheral/cranial neuropathy, myelitis), hematologic (immune thrombocytopenic purpura, autoimmune hemolytic anemia, thrombotic thrombocytopenic purpura), and cardiovascular (heart failure, myocardial ischemia, cardiac arrythmia, Libman-Sacks endocarditis). Multiorgan disease was defined as manifestations in ≥2 of the above organ systems. Self-reported race/ethnicity was categorized as White, Hispanic, Black, and Asian. Kaplan-Meier methods and log-rank tests compared organ system-free survival following SLE diagnosis by race/ethnicity; participants who did not develop outcome of interest were censored at their CLUES study visit. Cox proportional hazard models assessed the risks of end-organ disease by race/ethnicity, with age at diagnosis and female sex as covariates.
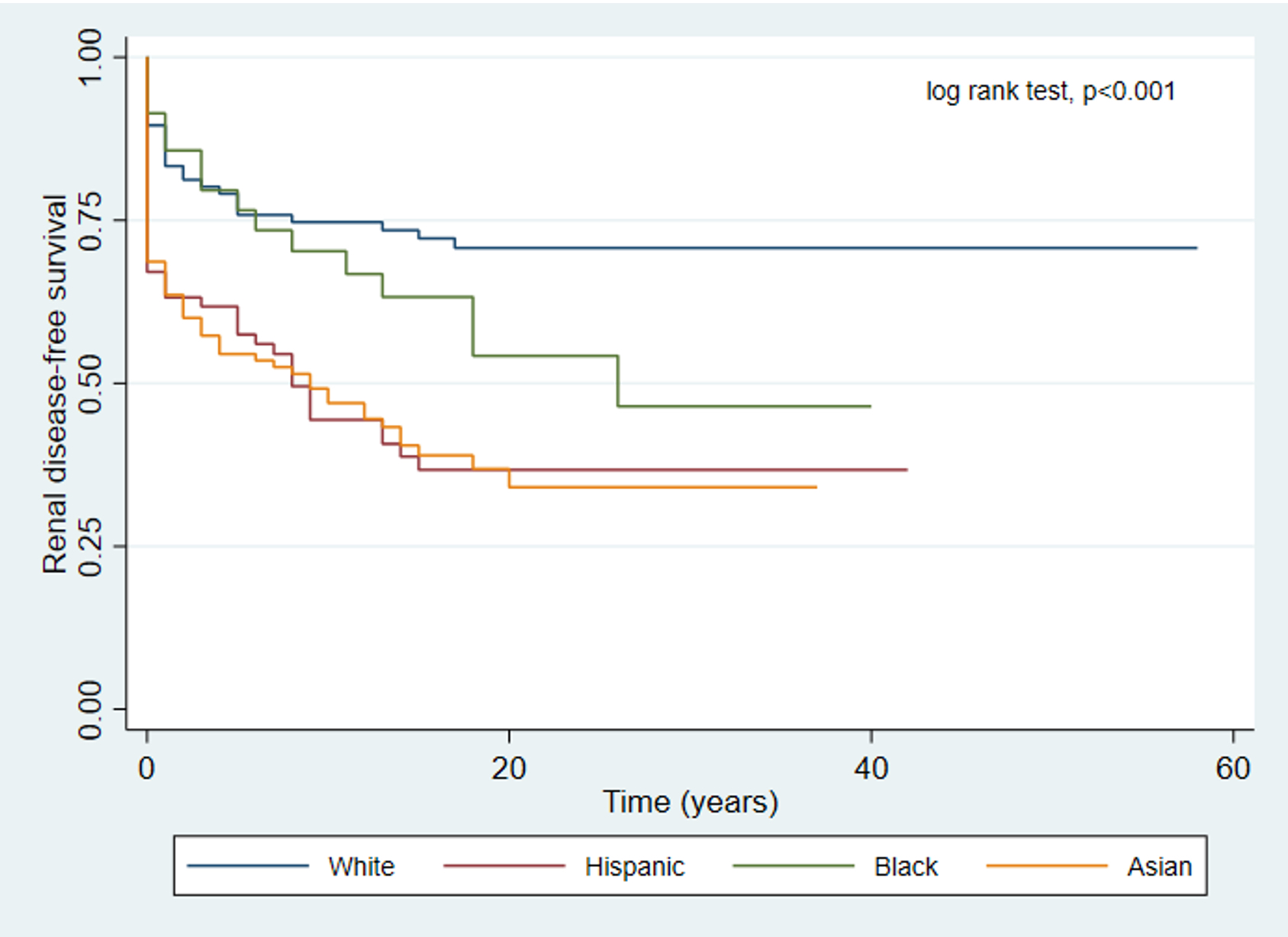
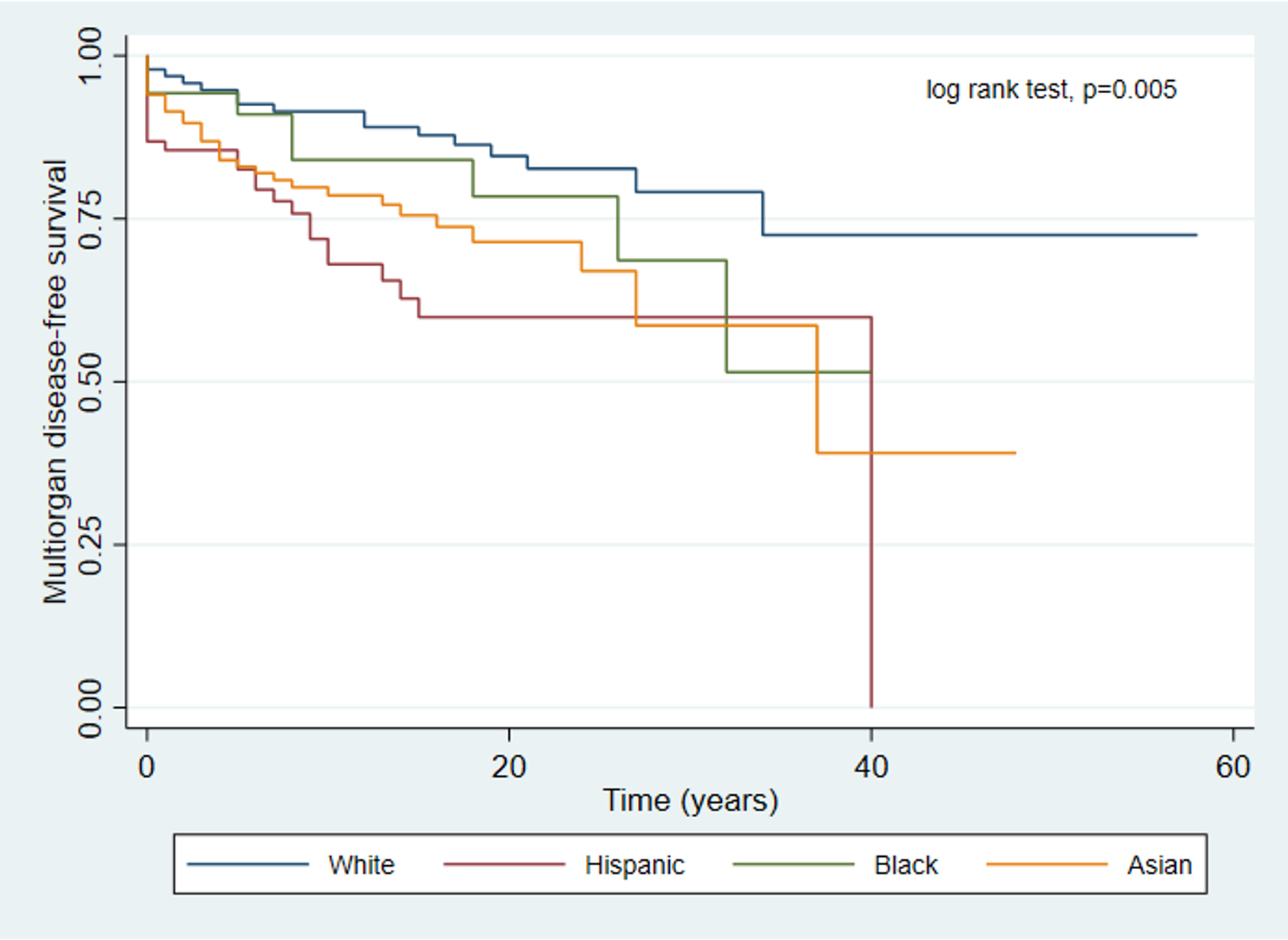
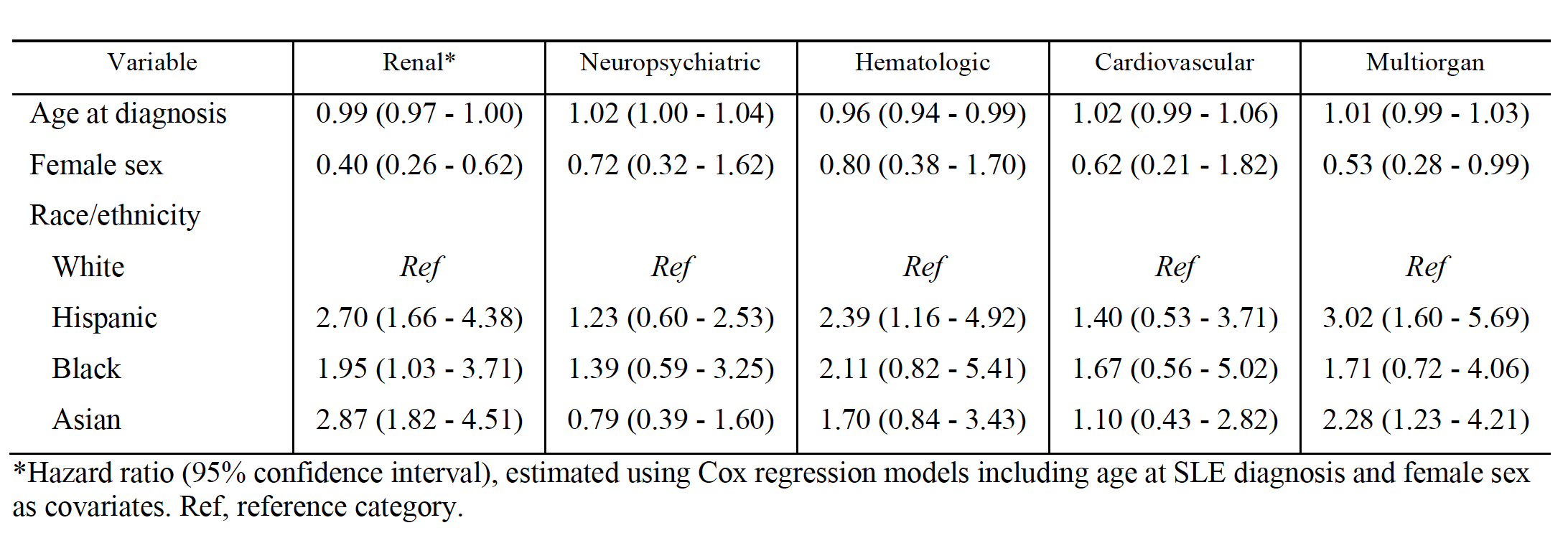
Results: CLUES participants are 89% female and have a mean age and age at diagnosis of 45 and 29 years, respectively. The distribution of self-reported race/ethnicity was as follows: 29% White, 23% Hispanic, 11% Black, and 36% Asian. Renal, neuropsychiatric, hematologic, cardiovascular, and multiorgan disease was confirmed in 154 (46%), 53 (16%), 62 (19%), 30 (9%), and 79 (24%) subjects, respectively. The median time to development of multiorgan disease was 9.5, 5, 8, and 3.5 years for White, Hispanic, Black and Asian subjects, respectively. Race/ethnicity was associated with significant differences in time to onset of renal and multiorgan disease (Figures 1 and 2). Cox regression models showed that non-White racial/ethnic groups experienced greater risks of renal, hematologic, and multiorgan disease as compared to White participants (Table 1).
Conclusion: Racial/ethnic minorities with lupus are at higher risk for developing end-organ disease as compared to White patients. Black patients experience higher hazards of lupus nephritis compared to White patients, although conclusions in other domains are limited by sample size. Our data highlight the risk of lupus nephritis and multiorgan disease among Hispanic and Asian patients, and hematologic manifestations among Hispanics, who experience these manifestations earlier in their lupus disease course as compared to White patients.
To cite this abstract in AMA style:
AGUIRRE A, Seet A, Trupin L, Katz P, Barbour K, Lanata C, Dall'Era M, Yazdany J. Racial and Ethnic Disparities in Risk of End-Organ Disease Following SLE Diagnosis in a Multi-Ethnic Cohort [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/racial-and-ethnic-disparities-in-risk-of-end-organ-disease-following-sle-diagnosis-in-a-multi-ethnic-cohort/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/racial-and-ethnic-disparities-in-risk-of-end-organ-disease-following-sle-diagnosis-in-a-multi-ethnic-cohort/