Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Acute low back pain (LBP) affects over 25% of adults annually in the United States, and as many as one-third of these individuals will develop chronic LBP. Many disparities in LBP exist, including this transition from acute to chronic LBP, with Black adults experiencing nearly twice the transition rate compared to White adults. Social determinants of health, such as race, are often associated with differences in health status and outcomes, with negative social exposures being associated with heightened systemic inflammation, immune cell activation, and prolonged recovery from health events. The purpose of this study was to examine if race was associated with immunological changes during the transition from acute to chronic LBP.
Methods: Adults experiencing acute LBP (pain < 4 weeks with no pain in the prior 30 days), were recruited from the community. Data was gathered at baseline and 3-month follow-up to determine the participant’s low back pain status (i.e., transition to cLBP). At both study visits, pain questionnaires and blood samples were collected, demographic characteristics were captured at baseline visit only. Peripheral blood mononuclear cell (PBMC) phenotyping and stimulation assays were used to test the differences between innate and adaptive immune status by race and transition status.
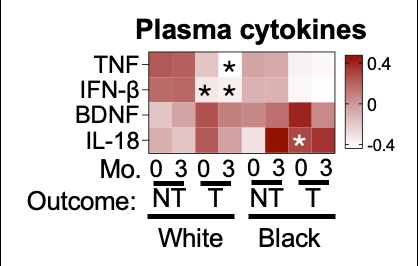
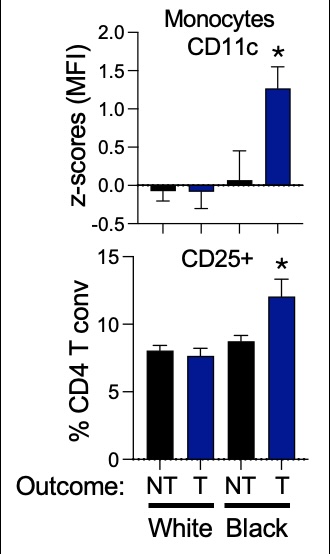
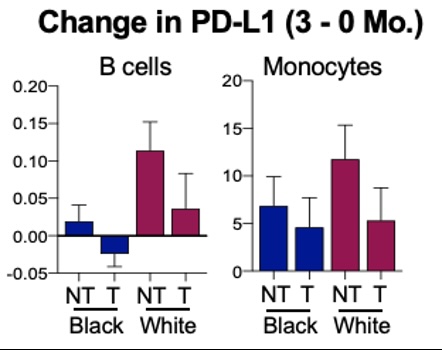
Results: Data was collected on 108 adults, of which 98 identified as White or Black/African American (69% white, 21.3% Black or African American), with a mean age of 58.98 years and approximately 60% female. Inflammatory plasma cytokine differences between those who transitioned to chronic LBP and those who did not transition were generally consistent between Black adults and White adults. Notably, the association of a subset of immune cell phenotypes with chronic LBP transition were race specific. Among these included plasma cytokine changes by race and transition status (Figure 1). CD11c on monocytes and CD25 (activation marker) on conventional CD4 T cells. Both markers were higher in those who transitioned to chronic LBP compared to those who did not transition to chronic LBP, but only in Black participants at baseline (Figure 2). Differences between changes in levels of B cells and Monocytes were noted based on transitioning to chronic LBP vs. not transitioning as well as differences by race, with White adults who did not transition having the greatest level of change in both B cells and Monocytes (Figure 2). Additionally, differences in PD-L1 on B cells and monocytes changes were greatest in White adults who do not transition to chronic LBP and lowest in Black adults who do transition to chronic LBP (Figure 3).
Conclusion: Immunological features are associated with race in the transition to chronic LBP. Racial disparities are observed in immunological features associated with the transition to chronic LBP. Changes in inflammatory responses are highest in White adults who do not develop chronic LBP. While race alone does not explain these differences, it points to the need for further investigation into how social factors influence the immune system leading to disparities in LBP outcomes.
To cite this abstract in AMA style:
Burke C, Brown M, Fillipo R, Danyluk S, Seebeck K, Goode A. Race-Based Differences in Immune Responses Following an Episode of Acute Low Back Pain Among Those Who Develop Chronic LBP and Those Who Do Not [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/race-based-differences-in-immune-responses-following-an-episode-of-acute-low-back-pain-among-those-who-develop-chronic-lbp-and-those-who-do-not/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/race-based-differences-in-immune-responses-following-an-episode-of-acute-low-back-pain-among-those-who-develop-chronic-lbp-and-those-who-do-not/