Session Information
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: The southern United States is home to a large proportion of non-Hispanic Black Americans, a group which has historically been disproportionately affected by healthcare disparities. Alabama in particular stands in the top quintile for both percentage of African American population and poverty rates. The COVID-19 pandemic has highlighted the impact of these disparities, particularly in those with rheumatic disease who, on average, already have a high utilization of healthcare services. A study nested within a voluntary U.S. physician registry showed poorer outcomes in racial/ethnic minority patients. However, data on socioeconomic status for registry patients was not reported. Our study examined the impact of race and socioeconomic status on COVID-19 outcomes in patients with rheumatic disease from a large tertiary care rheumatology practice in the Deep South.
Methods: We systematically identified rheumatology patients established at our medical center with a history of COVID-19 infection, confirmed by PCR. A retrospective medical record review was conducted to extract demographic characteristics, rheumatic disease type and treatment, comorbidities, and COVID-19 outcomes. COVID-19 outcomes studied included hospitalization, need for supplemental oxygen, need for mechanical ventilation, and death. Race/ethnicity was categorized as white, Black, or other. Census-tract socioeconomic status using area deprivation index (ADI) was calculated. Multivariate logistic regression was performed adjusting for the effect of age, sex, body mass index (BMI), comorbidities (by Charlson Comorbidity index), rheumatic disease type, rheumatic disease medications taken prior to COVID-19 infection, prednisone use prior to infection, and ADI.
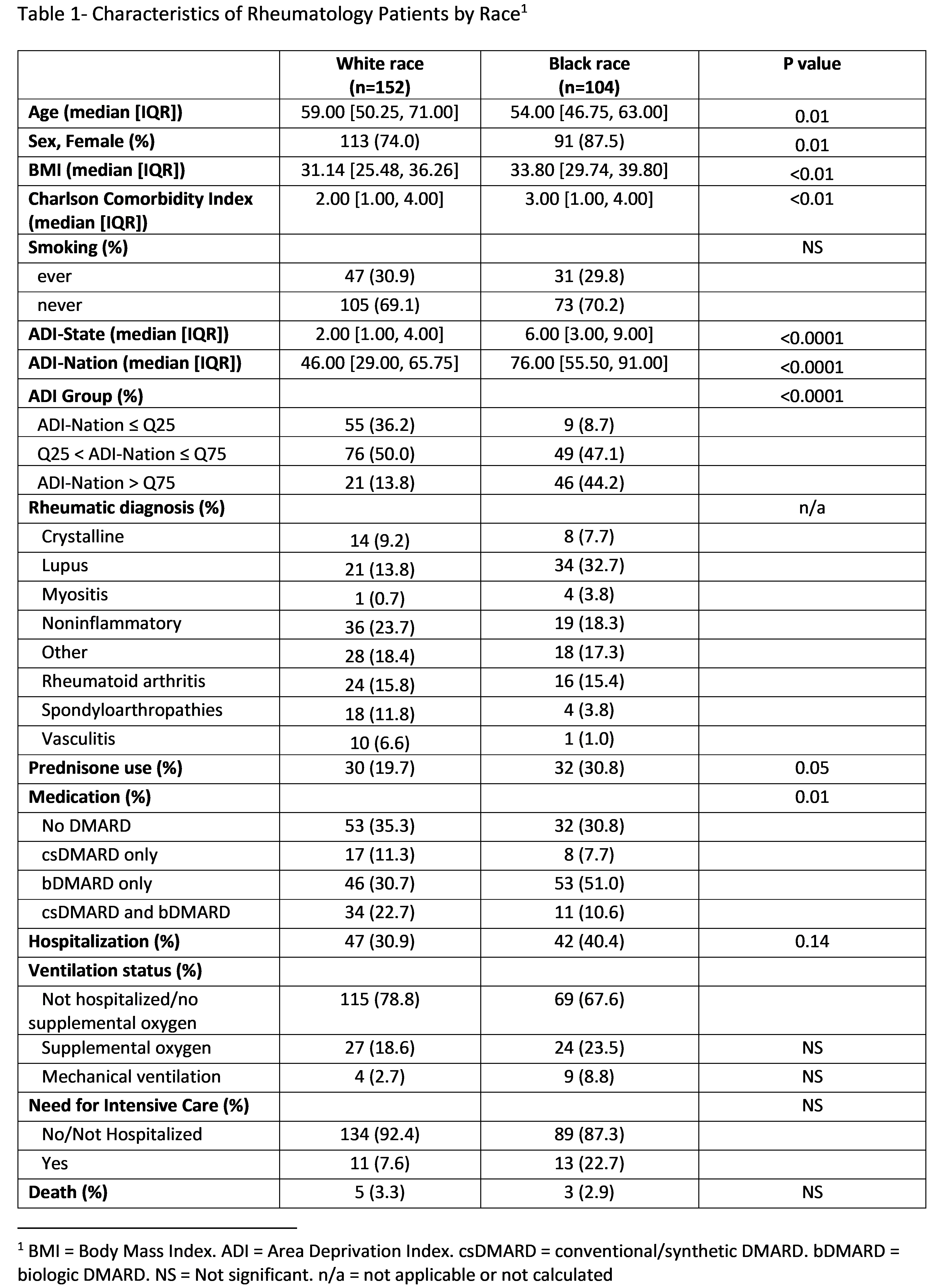
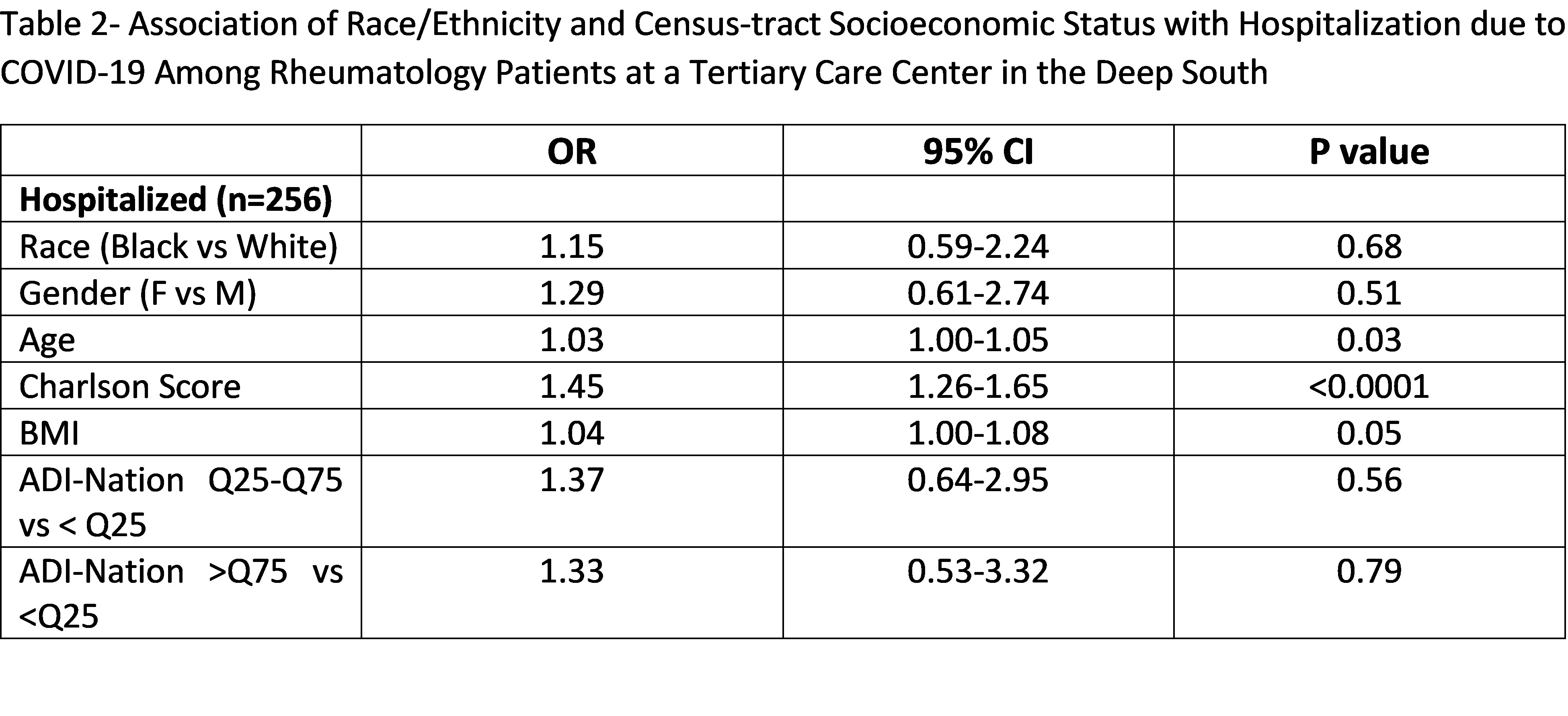
Results: A total of 256 rheumatology patients who had tested positive for COVID-19 at our institution were included, of whom 104 (40.6%) were Black and 152 (59.4%) were white (Table 1). Eight patients identified as “other” race were excluded from this analysis. Mean national area deprivation index for white patients was 46, while Black patients were more disadvantaged with a mean ADI of 76. Black patients also had higher baseline comorbidities and had a higher rate of hospitalization. However, after multivariate adjustment, Black race and ADI were not associated with hospitalization, need for supplemental oxygen, or need for mechanical ventilation. Variables noted to be significantly associated with hospitalization in multivariate analysis included age, BMI, and comorbidities (Table 2).
Conclusion: Although Black patients had a higher rate of hospitalization compared to white patients, race and census-tract socioeconomic status were not associated with significantly worse COVID-19 outcomes after accounting for confounders in this analysis. Possible explanations for these findings are lack of patient-level socioeconomic data, small sample size, and unmeasured confounding. Further investigation is needed to address this complex relationship between race and socioeconomic status and COVID-19 outcomes.
To cite this abstract in AMA style:
Taylor A, Sun D, Foster J, Danila M. Race and Socioeconomic Status and COVID-19 Outcomes in Patients with Rheumatic Diseases: Findings from a Tertiary Care Center in the Deep South [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/race-and-socioeconomic-status-and-covid-19-outcomes-in-patients-with-rheumatic-diseases-findings-from-a-tertiary-care-center-in-the-deep-south/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/race-and-socioeconomic-status-and-covid-19-outcomes-in-patients-with-rheumatic-diseases-findings-from-a-tertiary-care-center-in-the-deep-south/