Session Information
Date: Friday, November 6, 2020
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster I: Clinical Manifestations
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: The prevalence of SLE pulmonary involvement varies depending on several factors, including diagnostic methods. In this study, we sought to determine the frequency of involvement with different diagnostic methods in a single-center cohort.
Methods: 300 randomly chosen patients with SLE were included. Chest x-ray (CXR), lung spirometry, carbon monoxide diffusion test (DLCOc), and echocardiography were performed. High-resolution thorax computed tomography (HRCT) was done for a definite diagnosis of interstitial lung disease (ILD) whilst diagram electromyography (EMG), ultrasonography (USG), and magnetic resonance imaging (MR) were utilized to diagnose shrinking lung syndrome (SLS).
Results: 88,3 % of the cohort was female. The mean age and follow-up time were 43 and 11,5 years respectively. Of 300 patients, 16 % had ILD, 6,7 % had pulmonary hypertension (PHT), 3 % had SLS, 0,3 % had pulmonary infarction. At the start of the study, the prevalence of these involvements obtained from the patients’ records showed that 4 % had ILD, 5 % PHT, 0,3 % SLS, and 0,3 % pulmonary infarction. The median age, mean duration of disease, and follow-up time were significantly higher and longer in patients with ILD compared to patients without (p< 0.05). Forced expiratory volume (FEV1), forced vital capacity (FVC), DLCOc, and total lung capacity (TLC) were significantly lower in patients with ILD and with SLS (p< 0,001). Patients with ILD had a significantly higher frequency of arthritis, serositis, Raynaud myositis, and anti-Scl70 positivity. Neuropsychiatric damage, avascular necrosis, diabetes, and malignancy were significantly more frequent in those patients. All patients with suspected SLS has undergone diagram EMG, USG, and MR. Out of 10 suspected cases, in 6 EMG, in 5 USG and in 9 MR was compatible with SLS diagnosis(table 1). 5 patients had 3 of the diagnostic methods positive to diagnose SLS. Patients with SLS had a higher frequency of pleuritis, pericarditis, leukopenia, anti-Ro, and anti-La antibodies. Muscle atrophy and weakness, avascular necrosis were more frequent in this group of patients (p< 0.05). There were more patients treated with mycophenolate mofetil (MMF) and cyclophosphamide in the SLS group whilst more with MMF in the ILD group. Significantly higher frequency of patients had stopped using hydroxychloroquine (HCQ) in the ILD group (p=0,04).
Conclusion: Interstitial lung disease is common in patients with SLE and a considerable number of patients have SLS. Spirometry, diffusion tests, and chest x-ray are simple but valuable tools to shape a diagnostic approach for pulmonary involvement in patients with SLE. Diagram MR, USG, and EMG are complementary methods for a definite diagnosis in SLS. Considering the significant difference in prevalence between the start and the end of the study, one of the possibilities is the underrecognition of SLE pulmonary disease due to its being part of a multisystemic presentation. Moreover, the higher usage of immunosuppressives in these patients may support a multisystemic active disease. Although the drug effect is another concern, it is hard to establish a causal relationship due to the study’s cross-sectional design. HCQ may have a role in ILD prevention.
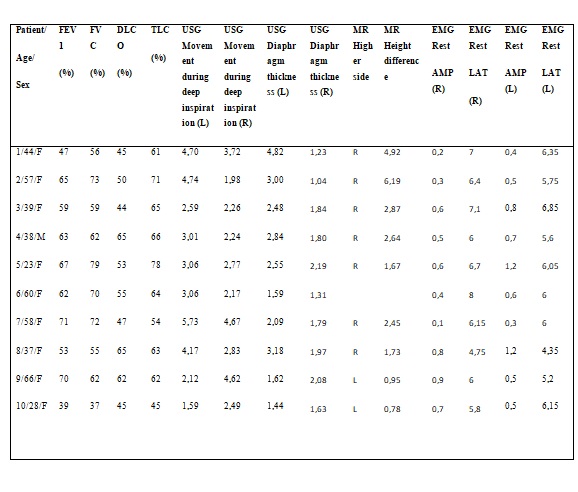 Table 1. Spirometry, DLCO, diaphragm EMG, diaphragm USG and MR results of patients with Shrinking Lung Syndrome.
Table 1. Spirometry, DLCO, diaphragm EMG, diaphragm USG and MR results of patients with Shrinking Lung Syndrome.
To cite this abstract in AMA style:
Senkal N, Kiyan E, Kocasoy-Orhan E, Demir A, Aydogan M, Yalcinkaya Y, Gul A, Inanc M, Öcal M, Artım-Esen B. Pulmonary Involvement in a Single Center Cohort of Patients with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/pulmonary-involvement-in-a-single-center-cohort-of-patients-with-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/pulmonary-involvement-in-a-single-center-cohort-of-patients-with-systemic-lupus-erythematosus/
