Session Information
Date: Sunday, November 17, 2024
Title: Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Dermatomyositis (DM) and polymyositis (PM) are idiopathic inflammatory myopathies characterized by muscles inflammation, proximal muscle weakness and extramuscular manifestations. A particularly challenging extramuscular manifestation of these myopathies is pulmonary hypertension (PH), which is often attributed to the development of interstitial lung disease in these conditions. There have been very few studies addressing PH in patients with DM and PM. We conducted a study to analyze pulmonary hypertension in hospitalized patients with dermatomyositis and polymyositis.
Methods: We analyzed the National Inpatient Sample (NIS) 2016-2021 for all hospitalized patients with DM and PM as primary or secondary diagnosis, dividing them into two cohorts: those with a concomitant diagnosis of PH, and those without a diagnosis of PH. ICD-10 codes were used to identify the diagnoses. We compared baseline characteristics, outcomes and healthcare utilization between the two cohorts. A p-value of ≤0.05 was considered statistically significant.
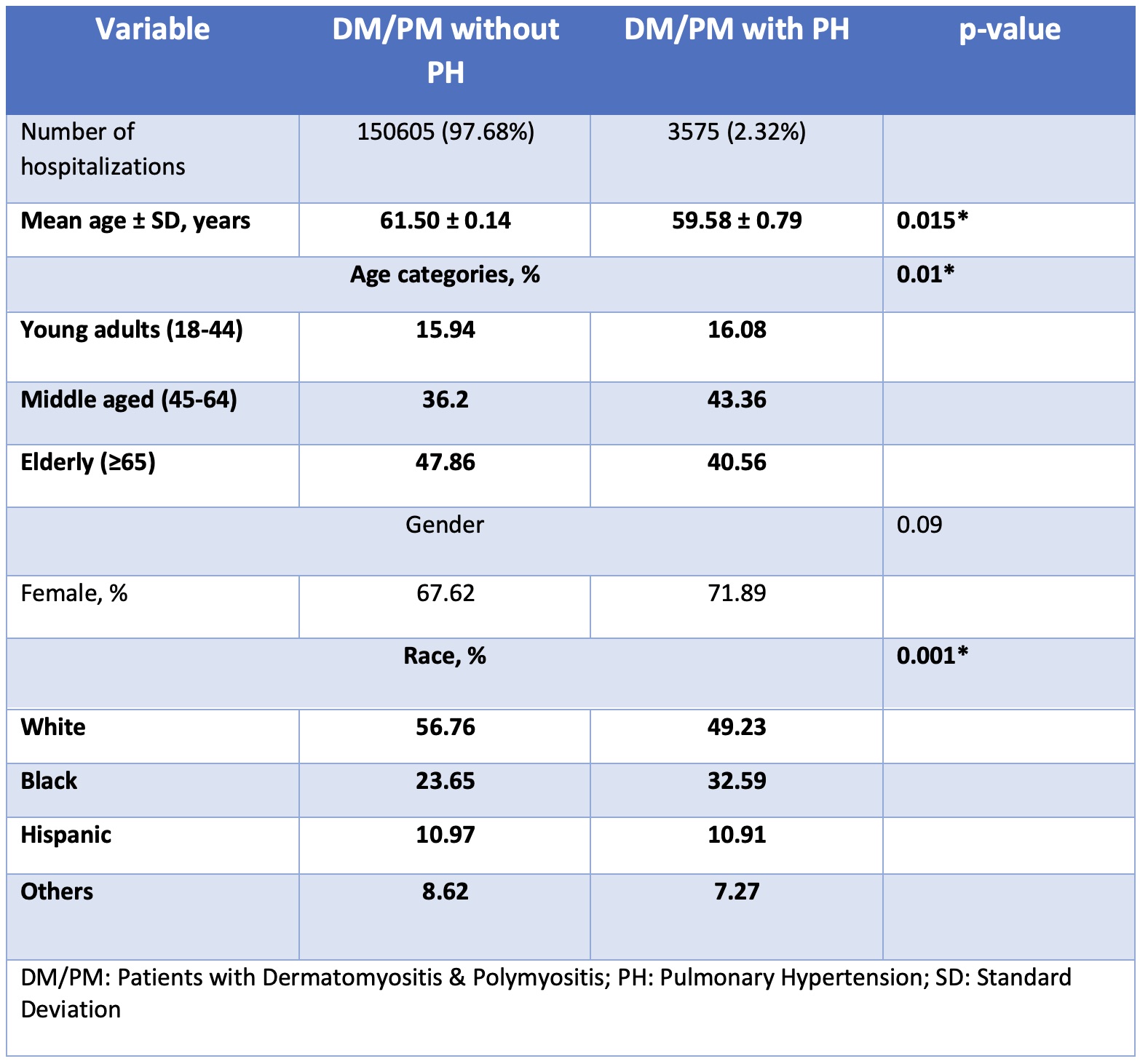
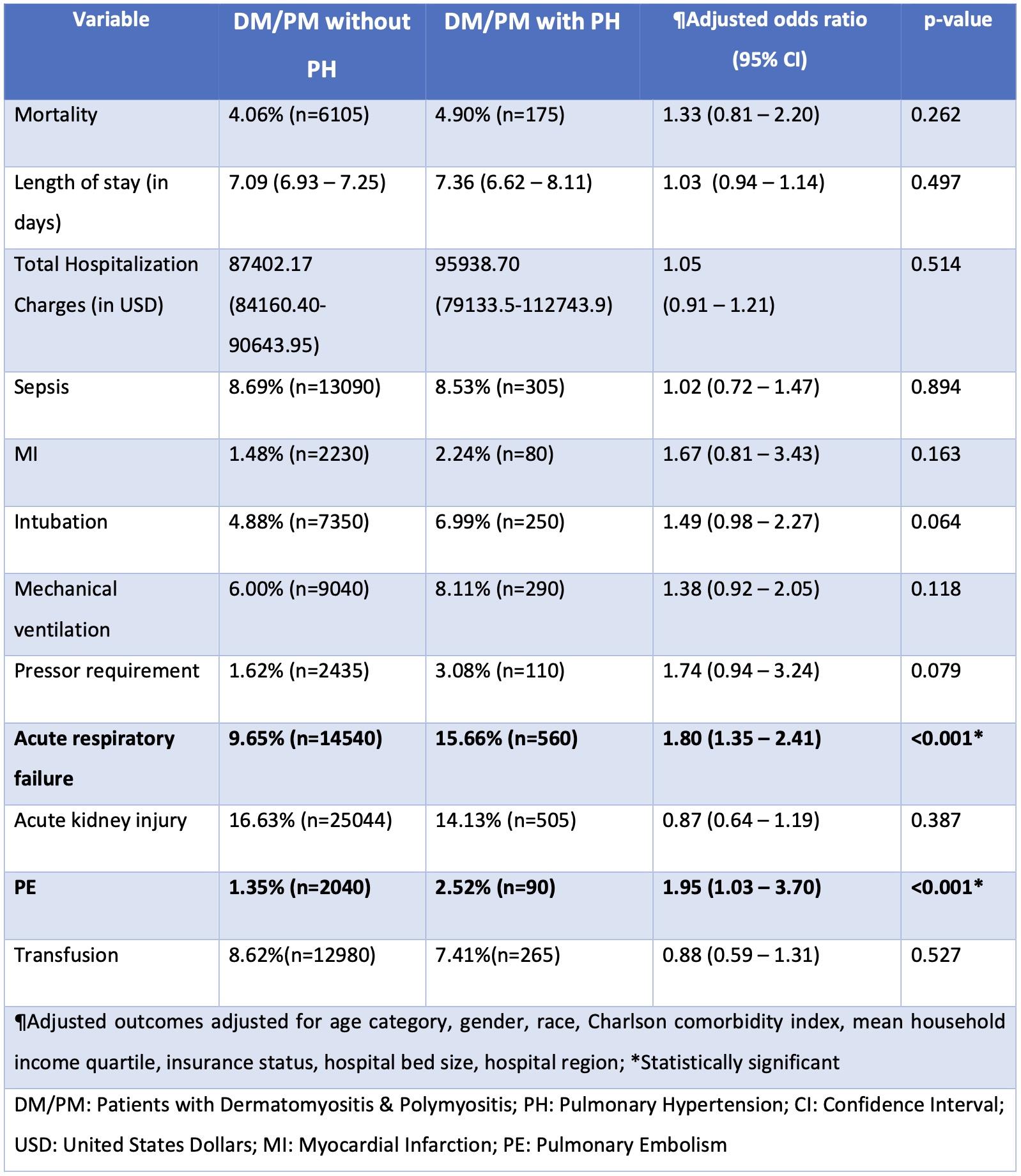
Results: From 2016-2021, a total of 154,180 patients with DM and PM were hospitalized, of which 3,575 (2.32%) patients had a diagnosis of pulmonary hypertension. When compared to hospitalized patients without DM and PM, hospitalized patients with these two diagnoses had 3 times higher odds of having pulmonary hypertension [OR: 3.01 p=< 0.001 (CI: 2.70 – 3.35)]. The cohort of patients with DM and PM who had concomitant PH had a slightly younger mean age (59.58 ± 0.79 years vs. 61 years ± 0.14, p= 0.015), a higher number of African American patients (32% vs 23.65%) and fewer white (49% vs 56%), Hispanic (10.91% vs. 10.97%) and other race (7.26% vs 8.26%) patients compared to the cohort without PH [p= < 0.001] (table 1). The PH cohort also had higher odds of developing acute respiratory failure (ARF) [OR: 1.8 (CI: 1.35 – 2.41) p=< 0.001] and pulmonary embolism (PE) [OR: 1.95 (CI: 1.03-3.70) p=< 0.001] during hospitalization. Among the two cohorts, there was no significant difference in odds of intubation, mechanical ventilation, acute kidney injury or sepsis. There was also no significant difference in mortality, total hospital charges or length of stay among the two cohorts (table 2).
Conclusion: The odds of having PH were 3 times higher in hospitalized patients with DM and PM compared to hospitalized patient without these diagnoses. Among hospitalized patients with DM and PM, there was a higher incidence of PH among African American patients compared to white, Hispanic and other race patients. Hospitalized patients with DM and PM who had PH also had higher odds of developing ARF and PE during their hospitalization compared to patients without PH.
To cite this abstract in AMA style:
Tanveer S, Ahluwalia D, Tanveer F, Saeed A, Razok A, Sami F. Pulmonary Hypertension in Hospitalized Patients with Dermatomyositis & Polymyositis: A Nationwide Cohort Analysis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/pulmonary-hypertension-in-hospitalized-patients-with-dermatomyositis-polymyositis-a-nationwide-cohort-analysis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/pulmonary-hypertension-in-hospitalized-patients-with-dermatomyositis-polymyositis-a-nationwide-cohort-analysis/